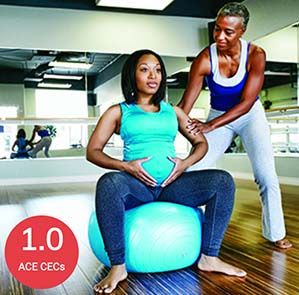
Pregnancy and Postpartum Exercise Training

We’ve come a long way since the days when women were urged to avoid any strenuous activity while pregnant (as if that’s even possible for women who already have children!). In the past several decades, a growing body of research highlighting the benefits of physical activity for both women and their babies has led to a significant shift in both attitudes and recommendations. In fact, unless a woman has a specific obstetric or medical condition that might prohibit activity, the likelihood of complications or a negative effect of either a single bout of exercise or a consistent training program is minimal.
That’s really good news for your clients who are pregnant (or even just thinking about it). To say that pregnancy is a time of great change, both physiological and emotional, is an understatement, but exercise has been shown to help ease this transition for many women. As a health and exercise professional, you have the opportunity to help guide your pregnant and postpartum clients in their efforts to stay active and enjoy the wide-ranging benefits of physical activity.
Physiological Changes During and Following Pregnancy
Pregnancy shepherds in a unique physiological timeframe during which a mother’s body undergoes numerous changes to safeguard the overall well-being of the fetus. Virtually every system is impacted by pregnancy, from cardiovascular to endocrine to metabolic. Some of these physiological adaptations are truly remarkable. For example, blood volume increases by 40 to 50%. Metabolic rate increases by 15%. Tidal volume increases by 30 to 50%. It’s important to remember, however, that all women will not experience the exact same changes or adaptations. Indeed, the rate and magnitude of adaptations are dependent on a complex interaction of genetics, individual health and exercise training/physical activity status.
The same is true after pregnancy, when various physiological changes follow different timelines in returning to pre-pregnancy levels. A cardiovascular change such as cardiac output, for example, typically returns to nonpregnant levels within several days, while other physiological adaptations, such as increased ventilation, persist for longer. Generally speaking, many physiological changes subside after four to six weeks.
Overall, designing safe and effective exercise programming for your clients requires that you understand the effects of pregnancy and the postpartum period on a woman’s physiological function, both at rest and during exercise. A list of key physiological aspects of pregnancy is presented in Table 1.
Table 1. Physiological Aspects of Pregnancy
|
System |
Parameter |
Change |
|
Cardiovascular |
Resting and Exercise Heart Rate |
↑ |
|
Resting and Exercise Blood Pressure (in 3rd trimester) |
↑ |
|
|
Blood Volume Blood Flow to Uterus |
↑ ↑ |
|
|
Endocrine |
Estrogen Growth Hormone Luteinizing Hormone Progesterone |
↑ ↑ ↑ ↑ |
|
Emotional/Psychological |
Depression Symptoms Lack of Emotional Stability Mood Fluctuations |
↑ ↑ ↑ |
|
Musculoskeletal |
Joint Laxity Balance |
↑ ↓ |
|
Metabolic |
Blood Lipids Body Weight Glucose Uptake to Fetus Water Retention |
↑ ↑ ↑ ↑ |
|
Respiratory |
Resting and Exercise Ventilation Resting Tidal Volume |
↑ ↑ |
Goals and Benefits of Exercise Programming
A careful collaboration between you, your client and her obstetric/medical provider can establish individualized goals for the exercise program. Following are some of the more common goals your clients might identify:
- Avoid excessive weight gain.
- Reduce the risk of gestational diabetes.
- Reduce the risk of hypertension.
- Lower the incidence of low-back pain.
- Reduce the incidence of psychological disorders, including postpartum depression.
- Prevent excessive decreases in cardiorespiratory and muscular fitness.
Preparticipation Health Screening
Regardless of current physical-activity levels, women with uncomplicated pregnancies should be encouraged to exercise. However, all pregnant women should be evaluated by their medical or obstetric care provider to determine whether exercise during pregnancy is contraindicated. Table 2 lists both absolute and relative contraindications to exercise during pregnancy, as identified by the American College of Sports Medicine.
Table 2. Contraindications to Exercise During Pregnancy
|
Absolute Contraindications |
Relative Contraindications |
|
Hemodynamically significant heart disease |
Anemia or symptomatic anemia |
|
Restrictive lung disease |
Cervical dilation |
|
Incompetent cervix/cerclage |
Unevaluated maternal cardiac arrhythmia |
|
Intrauterine growth restriction |
Chronic bronchitis or other respiratory disorders |
|
Multiple gestation at risk for premature labor |
Eating disorder |
|
Persistent second- or third-trimester bleeding |
History of spontaneous preterm birth, premature labor, miscarriage or fetal growth restriction |
|
Placenta previa after 26 to 28 weeks of gestation |
Poorly controlled type 1 diabetes |
|
Premature labor during current pregnancy |
Extreme morbid obesity |
|
Ruptured membranes |
Malnutrition or extreme underweight |
|
Preeclampsia/pregnancy-induced hypertension |
History of extremely sedentary lifestyle |
|
Severe anemia |
Mild/moderate cardiovascular disease |
|
Uncontrolled or poorly controlled hypertension |
Recurrent pregnancy loss |
|
Uncontrolled thyroid disease |
Orthopedic limitations |
|
Uncontrolled type 1 diabetes |
Poorly controlled seizure disorder |
|
Unexplained persistent vaginal bleeding |
Heavy smoker |
|
Other serious cardiovascular, respiratory or systemic disorder |
Other significant medical conditions |
It’s also recommended that you administer the Get Active Questionnaire for Pregnancy to prospective clients to help determine the appropriateness of participation in an exercise routine. The Get Active Questionnaire is designed to help exercise professionals and health coaches to identify the small number of women who should seek medical advice before continuing with or increasing physical activity during pregnancy and to address and overcome any concerns women may have about physical activity. It is also vital that you are knowledgeable of, and able to educate clients on, any potential signs that warrant the termination of exercise, including:
- Vaginal bleeding
- Abdominal pain
- Dyspnea prior to exertion
- Dizziness
- Headache
- Chest pain
- Muscle weakness
- Calf pain or swelling
- Amniotic fluid leakage
General Considerations for Pregnancy
Not surprisingly, fatigue, nausea and vomiting may limit a woman’s ability or desire to exercise, especially during the first trimester. As they move into the second trimester, their bodies require approximately 300 more calories per day to meet the increased nutritional and metabolic demands of pregnancy. While it is beyond your scope of practice as a health and exercise professional to provide specific nutrition recommendations to clients, offering them sound educational resources and information regarding the relationship between nutrition and a healthy pregnancy is not. Consider using these resources from the American College of Obstetricians and Gynecologists and the U.S. Department of Health and Human Services.
During pregnancy, women have diminished thermoregulatory control, so it’s important to encourage clients to maintain adequate hydration, wear appropriate clothing that helps disperse heat and avoid exercising in hot, humid conditions. Instead of exercising outdoors on a hot summer day, for example, choose environmentally controlled indoor settings, which offer a much safer and more comfortable environment for exercise during pregnancy. For more information on hydration and warm-weather clothing recommendations, check out Exercising Safely on a Warming Planet.
Cardiorespiratory Programming for Pregnancy
In general, the ACE Integrated Fitness Training® (ACE IFT®) Model guidelines for cardiorespiratory training can be applied to your clients during pregnancy and the postpartum period. However, the profound anatomical and physiological changes discussed earlier require that you make various modifications to different aspects of a cardiorespiratory-training program (Table 3).
The consensus statement for regular physical activity from the U.S. Surgeon General (30 minutes of moderate-intensity physical activity on most, preferably all, days of the week) is an appropriate target cardiorespiratory-training program for most women during uncomplicated pregnancies. Recreational and competitive athletes may train safely at higher intensities and volumes throughout pregnancy with the understanding that they undergo closer obstetric/medical supervision.
Table 3. Cardiorespiratory Programming Modifications for Women During Pregnancy
|
Program Component |
Program Modification |
|
Exercise mode |
Walking and cycling may be easier to monitor for exercise intensity. |
|
|
Activities that increase the risk of falls (e.g., skiing and skating), abdominal trauma (e.g., basketball and softball) or excessive joint stress (e.g., tennis) should be avoided and are generally not recommended. Activities at elevations greater than 6,000 ft (1829 m) and scuba diving are contraindicated. |
|
Exercise intensity |
Target heart rate (e.g., %HRmax or %HRR) should not be used to monitor exercise intensity due to the variability in maternal resting and HRmax throughout pregnancy. |
|
|
The talk test may be used to monitor appropriate exercise intensity. Pregnant women should exercise at an intensity that permits conversation. Intensity should be decreased when conversation is not possible. |
|
Exercise session duration |
Accumulating 30 minutes of exercise in 15-minute intermittent bouts may lessen energy balance and thermoregulatory concerns. |
|
Exercise frequency |
Moderate-intensity exercise should be regular rather than sporadic in nature. Exercise should be performed a minimum of three days per week, but preferably five to seven days per week. |
Note: HRmax = Maximal heart rate; HRR = Heart-rate reserve; adapted from the ACE Medical Exercise Specialist Manual
Resistance Training and Flexibility Recommendations for Pregnancy
In general, the ACE IFT Model guidelines for muscular training can be applied to clients during pregnancy and the postpartum period. However, several subtle adjustments that account for morphological and physiological changes will be required.
After the first 20 weeks of gestation, resistance and flexibility training exercises in the supine position should be avoided because of the potential obstruction of venous return and subsequent risk of orthostatic hypotension. Isometric or heavy resistance training may elicit a pressor response, which is a sudden increase in heart rate and blood pressure and is therefore not recommended. Joint range of motion is enhanced during pregnancy because of increased circulating levels of relaxin, which creates the potential for ligament and joint capsule damage with an overly aggressive flexibility program. For this reason, it is recommended to focus on helping clients maintain normal joint range of motion with slow, static stretching throughout pregnancy.
Programming for Low-back Pain and Other Biomechanical Considerations
The prevalence of low-back pain during pregnancy is high, with studies suggesting it ranges from 20 to 90%, with most studies reporting a prevalence greater than 50%. Other biomechanical issues during and after pregnancy include posterior pelvic girdle pain and pubic pain. Preventative programming is important to address these problems, as they can lead to inactivity and sedentary behaviors and, for some, an increased risk of psychological disorders. For instance, women with pregnancy-related posterior pelvic girdle pain are three times more likely to have symptoms of postpartum depression.
Programming for low-back pain and other pregnancy-related biomechanical issues should include a variety of posture, functional, mobility, and stretching-related exercises and movements. Here are some basic programming guidelines to consider implementing with your clients during pregnancy and the postpartum period.
Functional Exercises (12 to 15 repetitions of each)
Lower-extremity exercises:
- Single-leg squat
- Sit-to-stand squat
- Lateral lunge
- Single-leg hip abduction with band
- Single-leg lateral hip rotation with band
Upper-extremity exercises:
- Standing biceps curls
- Standing chest press
- Standing bilateral row
- Standing front overhead press
Core exercises:
- Bird dog
- Side plank
- Standing diagonal hay baler
Stretching exercises (hold each stretch at a point of slight discomfort for 15 to 60 seconds with continued breathing):
- Standing calf stretch
- Standing chest/shoulder stretch
- Standing, modified downward-facing dog
- Standing side bend
Postpartum Programming
Most women are able to gradually return to exercise if their delivery was uncomplicated. While the guidelines for postpartum exercise programming are generally the same as during pregnancy, there are several important considerations to be mindful of when working with your clients:
- Avoid exercise or physical activity that leads to undue fatigue and dehydration.
- Resume exercise slowly and progress gradually.
- Wear clothing and other apparel that supports the abdominal region and breasts. Women who are nursing may choose to feed their babies prior to exercise to alleviate the discomfort of engorged breasts.
- Pain is not a normal response to exercise and clients should stop if exercise is painful. Further, exercise should be stopped and medical attention sought if a client experiences bright red vaginal bleeding.
- Kegel exercises can be helpful for strengthening the pelvic floor.
- Postpartum depression impacts 15% of women after delivery. In the process of collaborating with your client, if you suspect that postpartum depression might be an issue, it is important to refer your client to her medical provider.
The ACE Mover MethodTM in Action: Help Clients Exercise Safely During Pregnancy and the Postpartum Period
As a health and exercise professional, you recognize that exercise throughout the lifespan, including during the gestational and postpartum timeframe, brings with it a myriad of health benefits. However, if your clients are unprepared or unaware of how to safely participate in physical activity, exercising during this time of life can bring discomfort and added risk of injury and health complications for mother and baby alike.
Are your clients knowledgeable about the various physiological responses to pregnancy? Do they know the warning signs of when to terminate exercise during pregnancy? What is the timeframe for resuming exercise postpartum? The ACE Mover Method is a great approach to asking open-ended questions that help your clients identify how they feel about their preparedness for exercise during and after pregnancy. Perhaps they have never exercised regularly and are unsure of how much or how intensely they should exercise, or what types of activity are best or contraindicated during pregnancy (see Table 3). Discuss any barriers that your client is encountering. For example, research suggests that respiratory discomfort (i.e., breathlessness) is present in approximately 75% of healthy pregnant women during regular activities of daily living. For this reason, you might need to reassure your clients that what they are experiencing is normal, and that subtle downward adjustments to exercise duration and intensity may be required to keep the physical activity tolerable.
Finally, collaborate and use your experience, research knowledge and what your clients share with you to come together and develop the best plan moving forward. Perhaps your client has mentioned that she is concerned about pelvic floor strength, but is unsure of where to start and, as a result, isn't doing anything to address it. Reassure your client that this is a common goal for many new mothers and set aside adequate time to review core and pelvic floor exercises. Collaborate with your client on identifying the exercises that she enjoys and feel comfortable performing, as well as on finding times in her busy (and likely sleep-deprived) schedule where these exercises, along with the entire training routine, can be completed.
Utilizing the ACE Mover Method sets you and your clients up for success because it helps them prepare for safe and effective exercise during and after pregnancy, which is especially important given the wide-ranging physiological and biomechanical changes that take place during this stage of life.
Expand Your Knowledge
Training for Prenatal and Postnatal Clients – Course Bundle
Helping prenatal and postnatal clients feel healthy, strong and equipped for motherhood is a fulfilling professional experience. It is also one that requires special knowledge and skills. Get a comprehensive overview of need-to-know information from the Training for Prenatal and Postnatal Clients course bundle so you can safely and effectively work with pregnant and postpartum women.
Oh Baby! Fitness® Pregnancy and Post-partum Exercise Instructor Training
Despite growing demand, there is a dearth of qualified health and fitness professionals who possess the specific knowledge and skill set to lead these crucial pre-and postnatal exercise programs. This training is for those who want to help new and expectant mothers regain strength and confidence, overcome postpartum depression, and forge a stronger bond with their child through the power of physical activity.