Cardiovascular disease (CVD) remains the leading cause of death in the United States, with an estimated 659,000 Americans dying of this disease each year, and a startling number of Americans (about 37.3 million) have diabetes, which often goes hand in hand with heart disease. Insulin resistance and prediabetes, which impacts one in three adults in the U.S., is a major risk factor for developing type 2 diabetes.
These numbers are both staggering and discouraging, but there is reason for hope. As a health and exercise professional, you know that lifestyle factors such as diet and exercise can significantly influence a person’s risk of developing CVD and type 2 diabetes. Lack of physical activity, a diet high in ultra-processed foods and habits such as excessive tobacco or alcohol use can directly impact one’s risk of developing diabetes and cardiovascular disease (Table 1). When clients improve their lifestyle habits, they can reduce their risk for CVD and insulin resistance.
So, where do you begin? How can you start coaching your clients to adopt healthier habits that will benefit their overall health and reduce their risk of both diabetes and heart disease? This article examines the modifiable risk factors for CVD, type 2 diabetes and insulin resistance, explains the common lab results that your clients may be receiving from their healthcare team, and offers insight into best practices for addressing lifestyle behaviors such as tobacco use and sugar intake.
Table 1
|
Risk Factors for CVD
|
Risk Factors for Insulin Resistance and Type 2 Diabetes
|
|
Having overweight or obesity
|
Having overweight or obesity
|
|
Being physically inactive (exercising less than three times per week)
|
Being physically inactive (exercising less than three times per week)
|
|
Consuming a diet high in ultra-processed foods and low in fruits, vegetables, healthy fats and whole grains
|
Consuming a diet high in ultra-processed foods and low in fruits, vegetables, healthy fats and whole grains
|
|
Using tobacco
|
Having a history of gestational diabetes
|
|
Being of African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian or Pacific Islander descent
|
Being of African American, Hispanic or Latino, American Indian, Alaska Native, Native Hawaiian or Pacific Islander descent
|
|
Having high blood pressure
|
Having a family member with type 2 diabetes
|
|
Having high cholesterol
|
Being age 45 or older
|
Research Review: How are CVD and Insulin Resistance Related?
A 2021 meta-analysis of 15 studies including almost 10 million individuals found that prediabetes is associated with an increased risk for heart failure. Fat cells are resistant to the effects of insulin and the resulting glucose uptake, which leads to more fatty acids and triglycerides being released. As a result, blood lipid levels increase.
Additionally, insulin resistance can lead to cardiovascular disease through atherosclerosis or hardening of the arteries, which is a result of high cholesterol and/or elevated triglycerides. Encouraging clients to get yearly physicals and preventive blood tests to monitor trends in their blood lipids and blood glucose levels over time is a great way to empower clients to remain in, or regain, control of and prioritize their health. Testing cholesterol is the only way to know if a person has high cholesterol, as there are no other symptoms. It is possible to improve lab levels with improved nutrition and physical activity, as well as by reducing smoking and/or excessive alcohol use.
Understanding Labs
It’s important to have a basic understanding of common terminology and lab tests, as clients may share their lab results with you or may have questions about interpreting values. However, this information is not for the purpose of diagnosing or treating a patient.
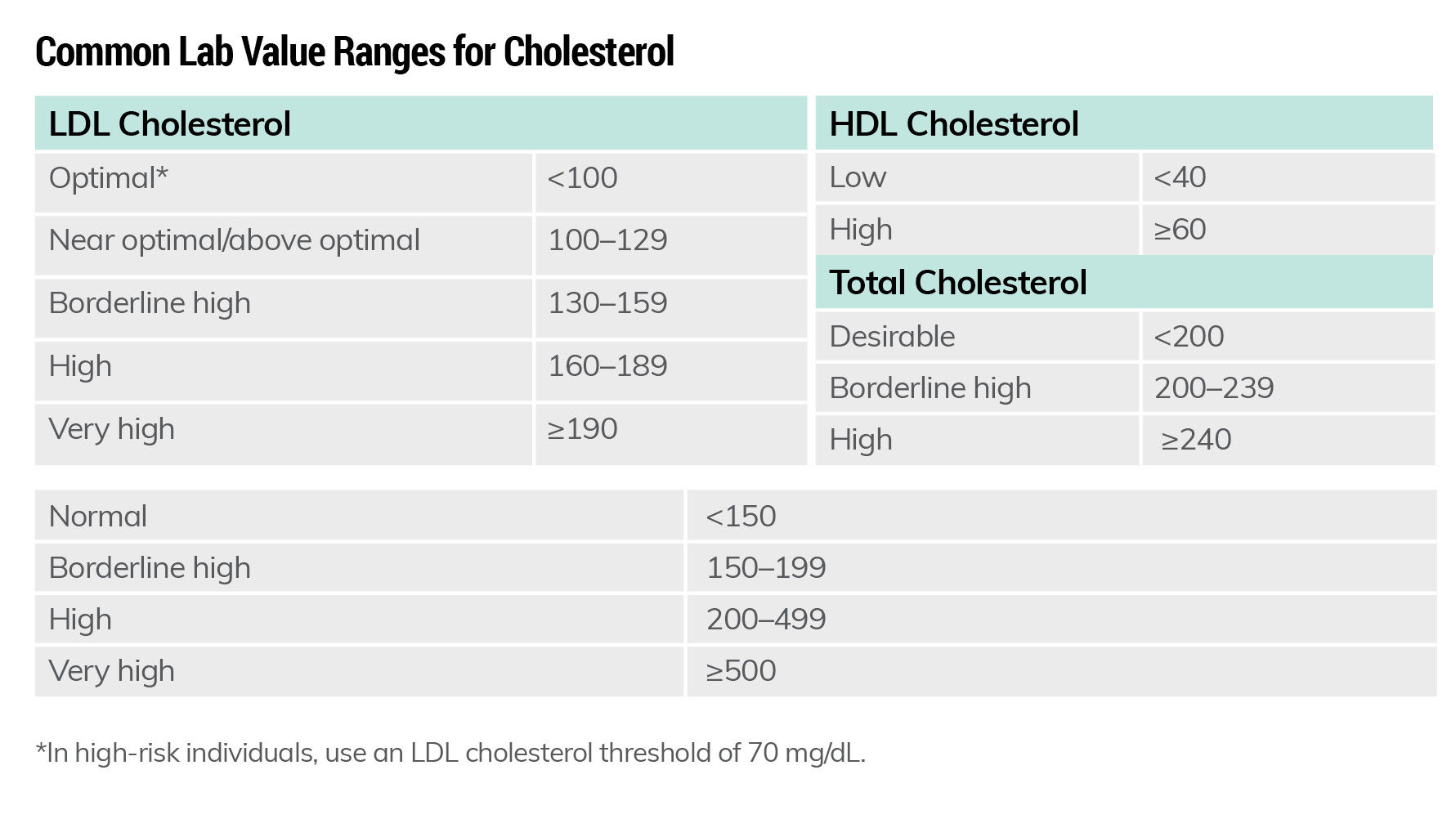
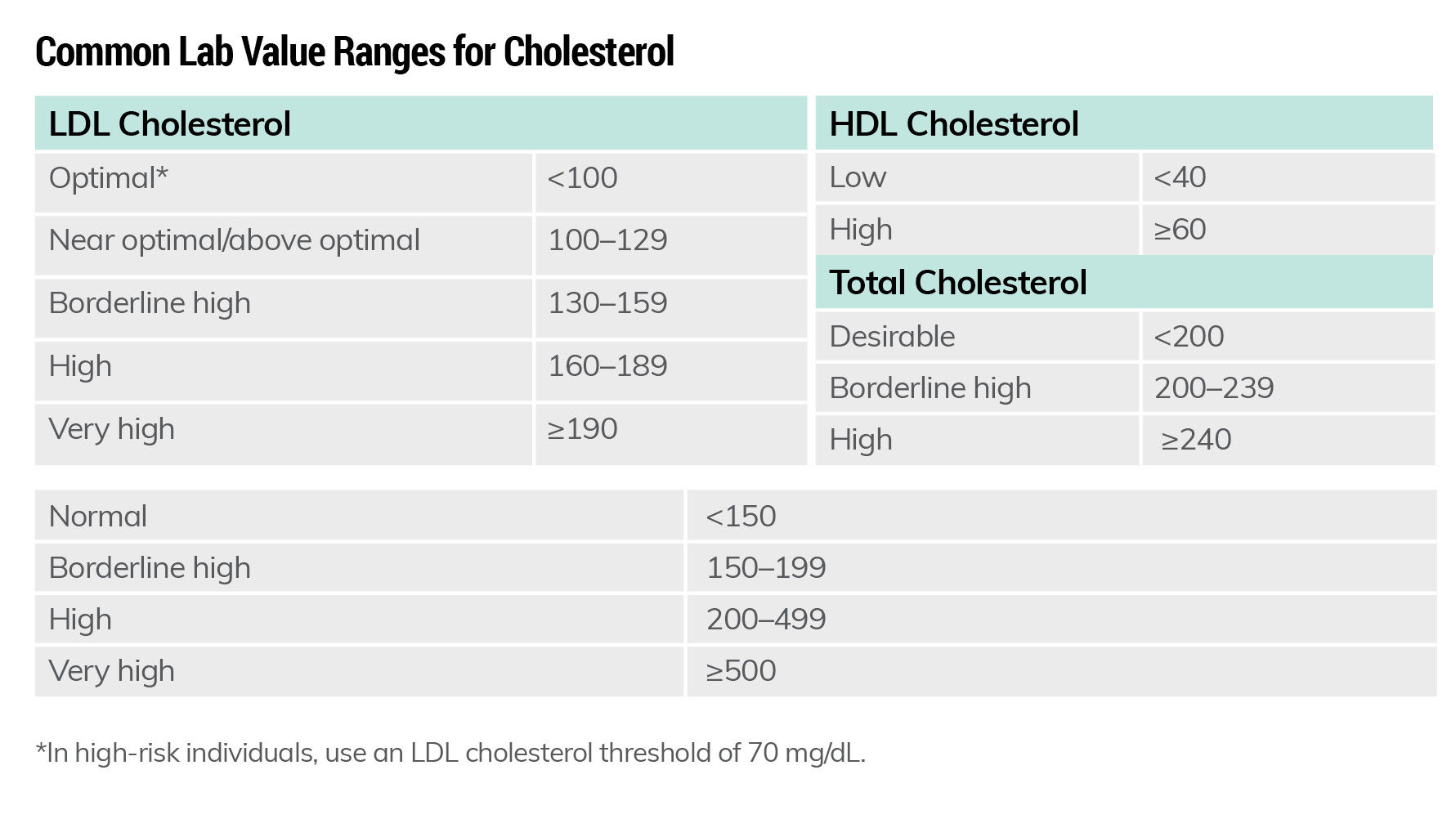
Blood lipids (cholesterol and triglycerides): There are two types of lipoproteins that carry cholesterol to the cells. Low-density lipoprotein (LDL) and high-density lipoprotein (HDL).
HDL: Known as the “good” cholesterol, this type of cholesterol is protective of heart health.
LDL: Often referred to as the “bad” cholesterol, this type of cholesterol contributes to fat build-up in the arteries and can cause atherosclerosis. High LDL levels increase an individual’s risk of heart disease.
Triglycerides: A type of fat. Excess fats consumed in the diet are stored as triglycerides. A high triglyceride level combined with low HDL and high total cholesterol levels can increase the risk of heart attack or stroke.
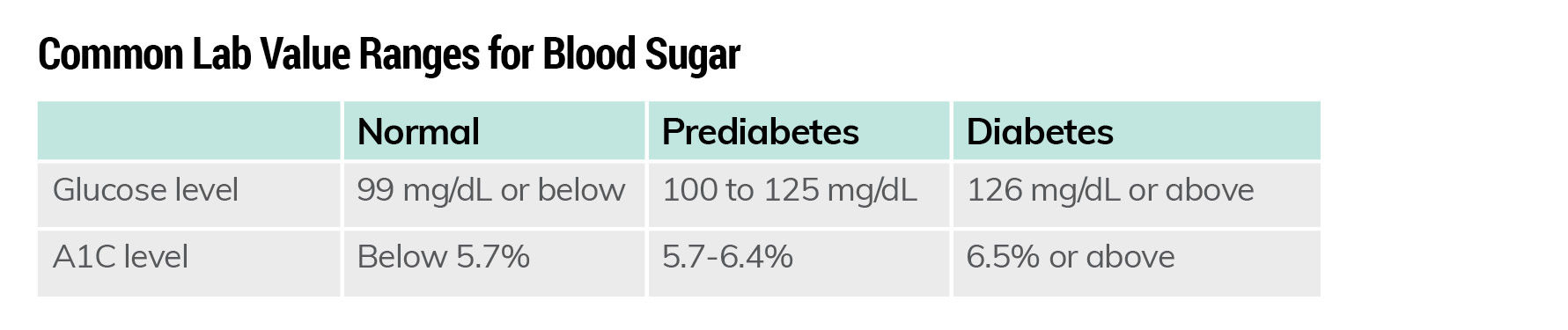
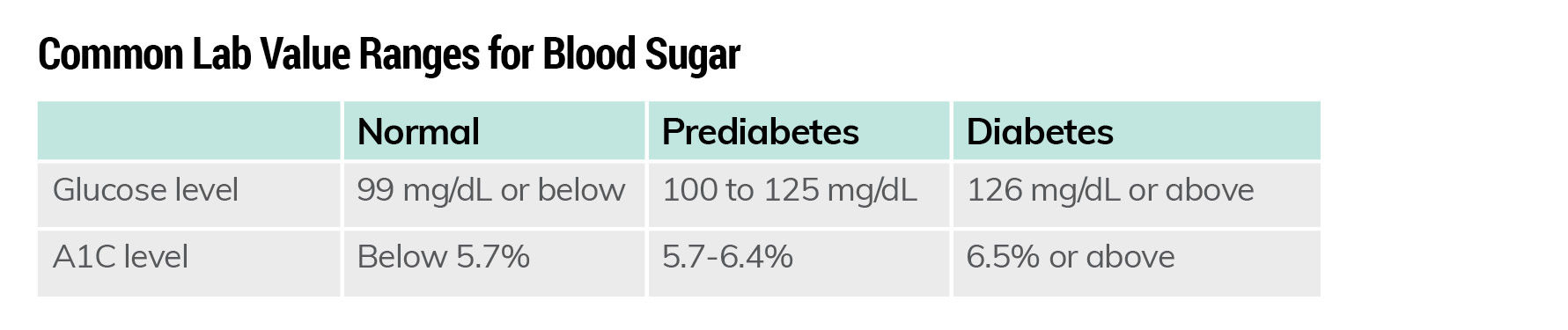
Blood sugar or glucose: Glucose is the the body’s preferred energy source. Blood sugar levels are typically assessed by A1C and glucose screening:
- A1C: This blood test for prediabetes/type 2 diabetes measures an individual’s average blood sugar levels over the past three months.
- Glucose screening: Measures the level of glucose (sugar) in the blood at a moment in time.
Applied Coaching: Evidence-based Lifestyle Interventions to Improve Labs and Reduce Insulin Sensitivity and Risk of CVD
While some risk factors for CVD are out of a person’s control (for example, age, family history, race or past cardiac events), there are several lifestyle habits and activities that are within a person’s control that can significantly improve health outcomes or prevent chronic diseases from becoming worse. The following evidenced-based strategies can be used to prevent a wide range of chronic diseases, including CVD and type 2 diabetes. They are also beneficial when incorporated into a prescribed medical intervention for clients who are at risk for, or have already developed, a chronic disease such as type 2 diabetes or CVD. It is essential that you always work in partnership with a client’s healthcare team.
1. Increase dietary fiber intake.
Research confirms that increasing dietary fiber intake by consuming fruits, vegetables, beans, seeds and whole grains can lead to improved heart health. Dietary fiber can reduce the risk of CVD by improving blood lipids, helping to manage blood pressure, and improving insulin sensitivity. While the average person eats about 15 grams of fiber per day, the recommended Dietary Reference Intake (DRI) for men is 38 grams per day and for women is 25 grams per day. Fiber intake should be increased slowly, however, as increasing it too quickly can cause gastrointestinal pain.
Offer your clients these practical tips for increasing fiber intake:
- Incorporate a fruit or vegetable at every meal or snack.
- Choose whole grains such as oats, whole-wheat bread, brown rice and quinoa as often as possible.
- Limit refined grained foods such as cookies, cakes, chips and crackers, which tend to be high in saturated fats, sugar and salt.
- Choose whole fruits rather than fruit juice.
- Eat beans and legumes.
- Keep chopped vegetables on hand for snacking.
2. Improve fitness levels.
Increasing physical activity can improve labs, increase insulin sensitivity and improve blood pressure, which reduces stress on the heart. A 30-year cohort study of patients with CVD found that physical-activity levels (and specifically not weight loss), was associated with a reduction in CVD mortality risk. The researchers concluded that physical activity needed to be both regular and sustained to confer the greatest cardiovascular benefits. They also found that any amount of activity was better than none.
While 150 minutes of moderate cardiorespiratory exercise combined with two sessions of muscular training per week is optimal, start where the client is at, and increase slowly. If a client has been diagnosed with CVD, work with the care team to make a plan for increasing physical-activity levels. Any amount of physical activity is beneficial and helping clients to find an activity they enjoy is key.
Here are some easy ways your clients can start becoming more physically active throughout the day:
- Start with small bouts of exercise throughout the day. Set timers or reminders for walking breaks.
- If a client feels bored during exercise, encourage them to listen to podcasts or music or to talk on the phone while walking or using cardio machines.
- Urge clients to create an environment that supports new habits by having their workout clothing and shoes set out or packed and ready to go.
- Remind clients to occasionally break up their routine by skipping their usual walking trails or paths and picking an alternative route or location.
- Whenever possible, encourage clients to exercise with a friend. Social support is extremely beneficial in building habits.
- Start sessions with the exercise the client enjoys most.
- Help clients work up to getting a combination of muscle building and cardiorespiratory exercise for optimal health and fitness improvement.
3. Reduce intake of sugar-sweetened beverages.
A 2020 study published in the Journal of the American Heart Association revealed a link between consuming one or more sugar-sweetened beverages per day and an increased risk of CVD and stroke. For this reason, helping clients reduce their sugar intake by limiting or eliminating sugar-sweetened beverages can have a significant impact on their overall health.
Regular consumption of sugary drinks, whether in the form of sodas, sweet teas, coffee drinks or smoothies, can be a tough habit to break, but it can be done. Here are some ideas to offer your clients:
- Encourage clients to replace their sugary drinks with sparkling or flavored waters. Having something besides regular water can help minimize the tendency to feel like they’re depriving themselves of a “treat,” while also helping them to stay hydrated.
- Set small, specific goals for reducing sweet drinks. Together with your client, develop a plan for weaning off sugar-sweetened beverages. For example, if a client is drinking a 20-ounce soda every day, they could start by choosing a smaller-sized drink. From there, they could opt to have a soda every other day instead of daily. For drinks like sweetened coffee or tea, they could opt for less sugary options, or reduce the amount of sugar they add to them. Over time, tastebuds may adapt and develop a preference for less-sweet drinks. (Note: Using the Bonus Tool button at the top of the page, ACE Certified Professionals can access and download a sample behavioral contract that can be used to help clients make positive lifestyle changes and stick with them over time.)
4. Reduce ultra-processed food intake.
Ultra-processed foods such as packaged chips and crackers provide little nutritional value and typically are high in added sugars, saturated fats and/or sodium. These foods are not filling, and they are easy to overeat without feeling satisfied. A 2019 clinical study highlighted the importance of reducing ultra-processed foods in the diet in favor of more satiating whole foods. Study participants consumed either ultra-processed or unprocessed diets (which included the same number of calories, energy density, macronutrients, sugar, sodium and fiber) for two weeks, and then switched diets. Participants were instructed to eat as much or as little as they wanted. On average, those eating ultra-processed diets consumed approximately 500 more calories per day and gained 1.3 to 2.6 pounds (0.6 to 1.2 kilograms) over the course of two weeks. In contrast, those eating the unprocessed diet lost an average of 1.3 to 2.6 pounds (0.6 to 1.2 kilograms).
Research such as this supports the idea that a nutrient-dense, balanced diet is most effective in terms of weight loss and health. Here are some ways your clients can begin to make the switch from an ultra-processed diet to a less-processed, more nutritious way of eating:
- Make the healthy choice the easy choice by keeping chopped fruits and vegetables in the house. Also, be sure to stock up on foods that are high in lean protein, healthy fats and high in fiber, as these help to increase satiety and reduce feelings of hunger throughout the day.
- Plan ahead. Help your clients learn how to make shopping lists, plan meals and do food prep ahead of time. When healthy food is readily available, it’s much easier to make a healthy choice.
- Avoid the diet mentality. Rather than completely cutting out all ultra-processed foods, encourage clients to identify the foods they love most as well as those they don’t care about. Next, help them create a plan for incorporating those favorite foods (for example, having ice cream on Wednesday and Friday nights).
Tobacco Cessation—Best Practices for Coaches
You don’t have to be a smoking-cessation expert to help clients quit using tobacco. Take the time to familiarize yourself with programs and available treatments in your area so you can provide clients with resources to support them on their journey to quit using tobacco. Here are some approaches you can use to support clients in their quest to stop smoking or other tobacco use:
- Utilize motivational interviewing to understand client motivation and stage of change. Ask questions to help the client explore the risks and rewards of smoking versus quitting.
- Connect clients with their health insurance provider, which may provide a free program. Many states offer free smoking-cessation programs as well.
- Medications are available to help people quit smoking. Refer clients to their primary care provider to explore the best option for them.
- Refer patients to the 1-800-QUIT-NOW (1-800-784-8669) Quit Smoking Hotline, the text messaging service SmokefreeTXT, the quitSTART app (iOS and Android) provided by smokefree.gov or other counseling resources.
- The Centers for Disease Control and Prevention also offers quitting information and resources.
5. Reduce smoking and excessive alcohol intake.
Smoking and excessive alcohol intake can exacerbate heart issues. Moderate drinking is defined as an average of one drink (12 ounces of beer, 4 ounces of wine or 1.5 ounces of 80-proof spirits) per day for women and one or two for men. Any amount of smoking is unhealthy. See information below about how to support clients who want to quit smoking. Note: If a client is experiencing alcoholism, this is outside your scope of practice. While you may certainly provide support, a more robust program is necessary for treating a person with alcohol use disorder.
Here are some helpful tips for those who want to reduce their alcohol intake:
- If a client wants to reduce their alcohol intake, help them develop a plan and follow up with them during the time of day they tend to reach for a drink. Numerous apps are available that can help an individual make intentional goals related to drinking alcohol and to track their daily and weekly consumption.
- Talk through a client’s reasons for drinking (these may include social reasons, wanting to “wind down,” or even unconscious habit), and then address alternative solutions. This might include ordering a different type of drink or drinking a mocktail on some nights, not keeping certain types of alcohol at home, practicing other stress-relieving strategies or only drinking on certain nights of the week.
- Clients may not know the nutritional implications of drinking, as alcoholic beverages are not required to list calories on their labels. Alcohol contains 7 calories per gram (almost as much as fats at 9 calories/gram), which adds up quickly, especially if consuming mixed drinks or having multiple drinks per day.
There are multiple ways to improve the risk for CVD and type 2 diabetes and associated lab values. Starting with what the client feels most confident in working on can help to build traction and create habits that stick.
Expand Your Knowledge
 |
As an ACE Fitness Nutrition Specialist, you’ll help your clients make healthier, long-lasting food choices through nutrition education and behavior change.
|
 |
Master the science of nutrition and the art of behavior change coaching with this practical nutrition course.
|
 |
This course bundle will equip you with information and meaningful behavior-change techniques to help you support your clients in healthier food choices and implement into your practice immediately.
|





 by
by