By Elyza E. Montano, M.S., Jamie M. Keith, Christina A. Buchanan, Ph.D., and Lance C. Dalleck, Ph.D., with Daniel J. Green
Fitness levels decline as people grow older due to both physiological and behavioral factors (Hoeger et al., 2018). Physiological factors involved in this decline include changes in the structure and function of the heart, lungs and muscle fibers (Karavidas et al., 2010; Morley et al., 2010), while the behavioral factors include physical inactivity/sedentary living, poor diet, tobacco use and alcohol consumption.
The health-related components of physical fitness—cardiorespiratory fitness, muscular fitness, body composition and flexibility—are all adversely affected by the aging process. Maximal oxygen uptake (VO2max), muscle strength and mass, and flexibility are all reduced, while total body mass and fat mass increase (Tuna et al., 2009). Collectively, these changes increase the risk of cardiovascular disease, metabolic disease, obesity, insulin resistance, back pain, fall risk and all-cause mortality, and reduce the ability to perform activities of daily living and maintain overall independence.
While these changes occur with advancing age, they can all be slowed by being physically active. But do older adults respond to exercise training in a way that is similar to their younger counterparts? ACE enlisted the help of Dr. Lance Dalleck and his team of researchers in the High Altitude Exercise Physiology Program at Western State Colorado University to find out.
The Study
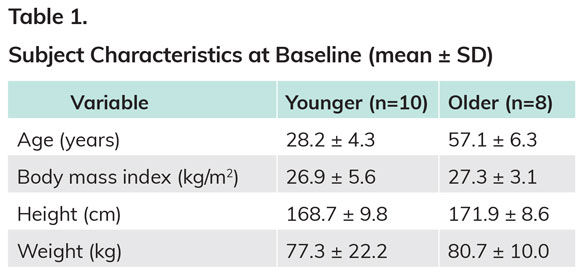
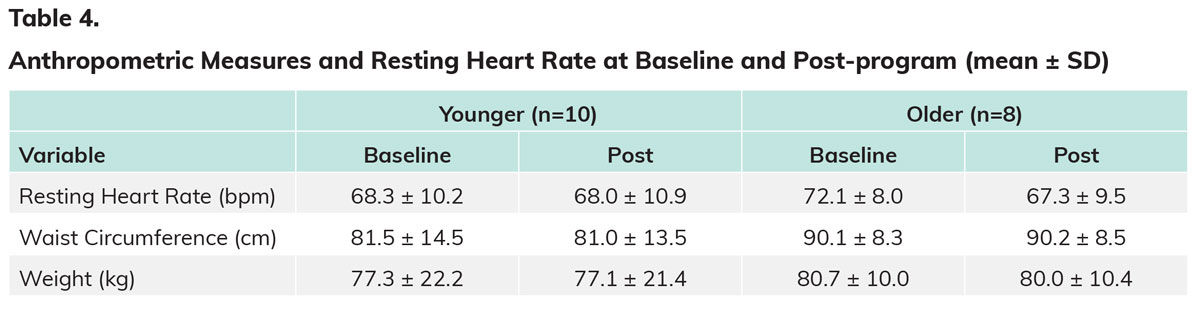
The researchers recruited 26 sedentary, low-to-moderate risk men and women to participate in this study. Eight participants dropped out of the study due to illness, personal matters or injury outside of the program, meaning that 18 people completed the study. Ten of those individuals were in the “younger” group (i.e., 18 to 35 years old), while eight were in the “older” group (i.e., 50 to 65 years old) (Table 1). All the women in the older group were postmenopausal.
Participants attended four sessions for baseline testing.
- Session 1: Subjects completed quality-of-life surveys, signed informed consent forms and became familiarized with the program commitment.
- Session 2: Fasting blood lipids, blood pressure (BP) and resting heart rate (HR) were measured.
- Session 3: Baseline testing was conducted, including VO2max, skinfold testing and flexibility testing, as well as height, weight and waist circumference measurements.
- Session 4: Five-repetition (5-RM) testing was completed for the leg press and bench press to measure muscular strength.
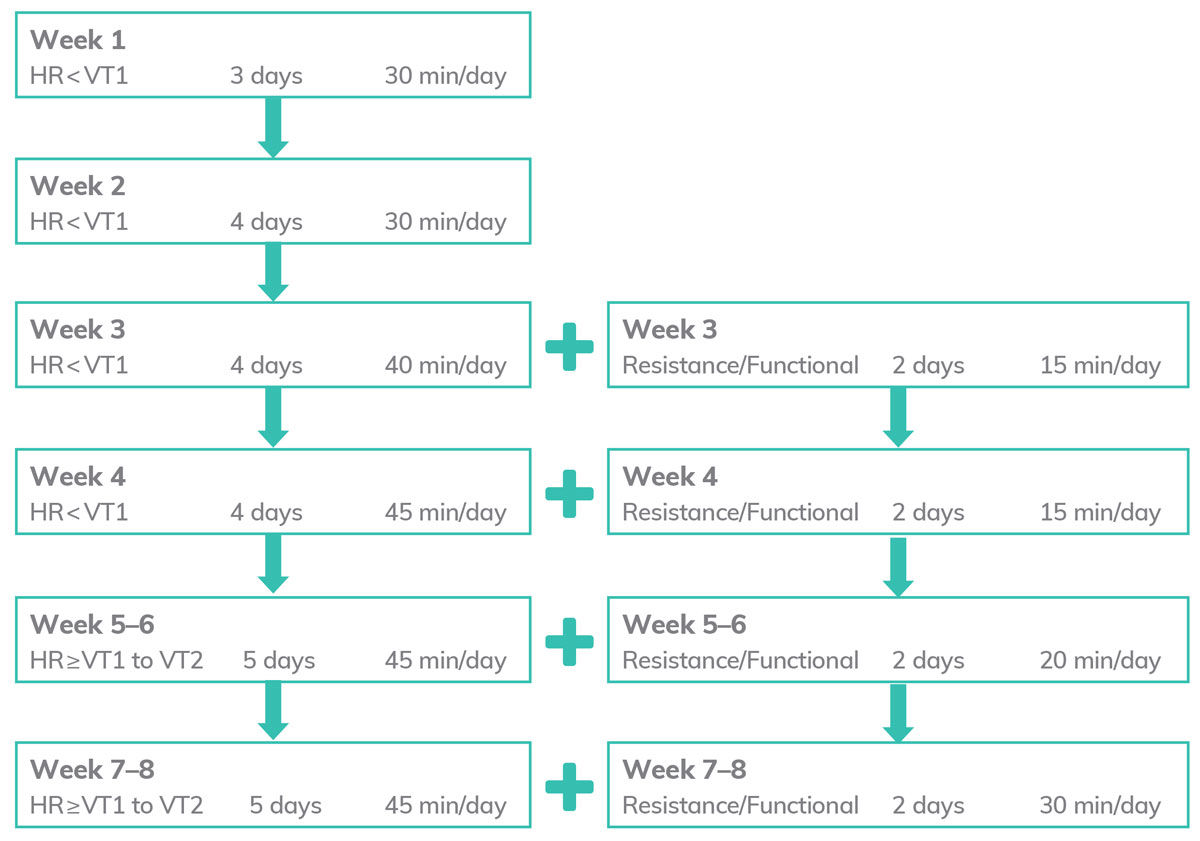
After this baseline testing was complete, participants completed an individualized eight-week exercise program created by the research team following the ACE Integrated Fitness Training® (ACE IFT®) Model. Phase 1 of the program covered weeks 1 through 4, with participants exercising three or four times each week for 45 to 60 minutes each day. Phase 2 included weeks 5 through 8, with participants exercising five times each week for 60 to 75 minutes each day.
All participants performed specific functional, resistance and cardiorespiratory exercise recommended for each phase of the ACE IFT Model (ACE, 2014). Following the eight-week program, all baseline measurements were repeated.
A Closer Look at the Exercise Program
A key element of this research, as with the ACE IFT Model itself, is that the exercise programs were individualized. To accomplish this, the researchers determined each participant’s first and second ventilatory thresholds (VT1 and VT2) and then used those values to program aerobic exercise intensity.
During weeks 1 through 4, aerobic exercise was performed at an intensity below VT1, while aerobic exercise during weeks 5 through 8 was performed at an intensity between VT1 and just below VT2. Participants wore HR monitors during all exercise sessions and workloads were adjusted to meet target HR values. They were able to choose among exercising on the indoor track, treadmill, recumbent bike, upright bike, elliptical, stair stepper or rower.
Resistance training was incorporated into the program during week 3. Subjects were monitored for safety, technique and progression as outlined in the ACE IFT Model. The muscles targeted were the hamstrings, glutes, quadriceps, triceps, shoulders, chest and back.
The full program is outlined in Figure 1.
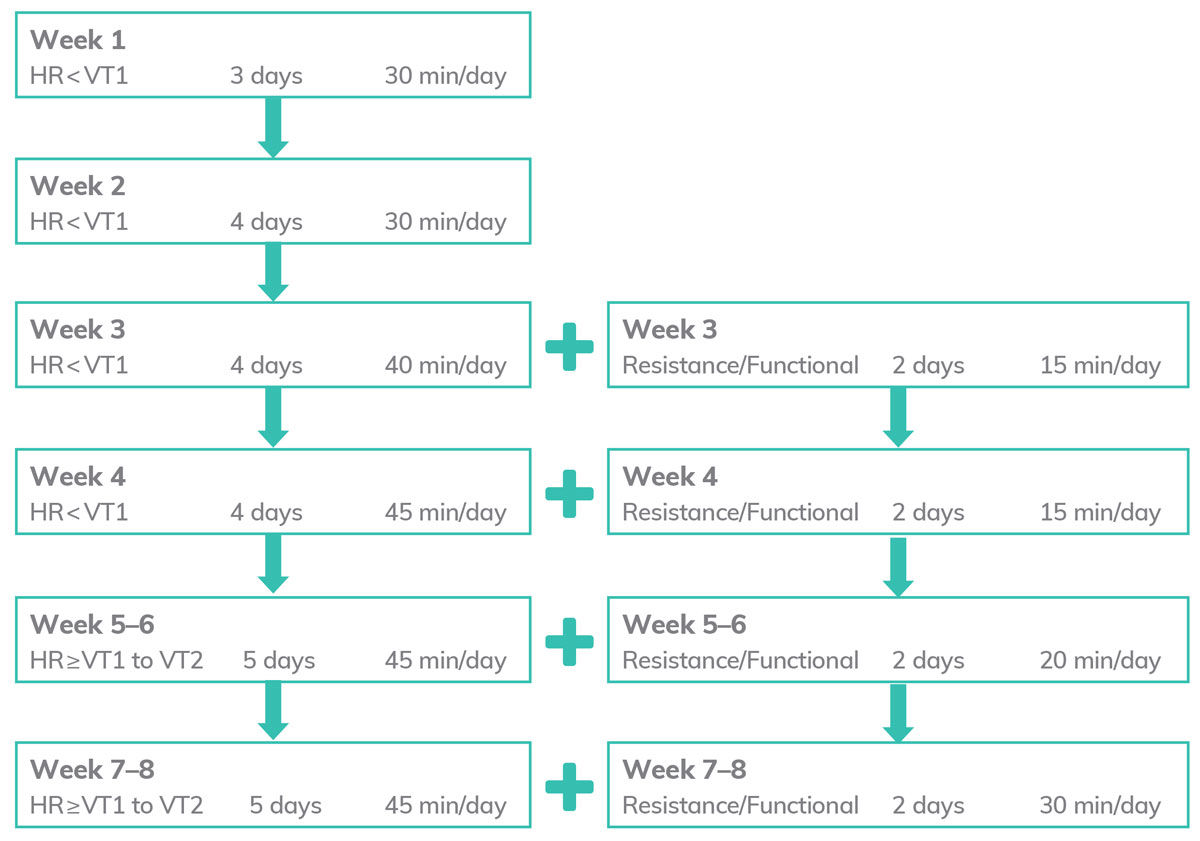
Figure 1. Week-to-week Exercise Program for Days/Times of Aerobic and Resistance Training
The Results
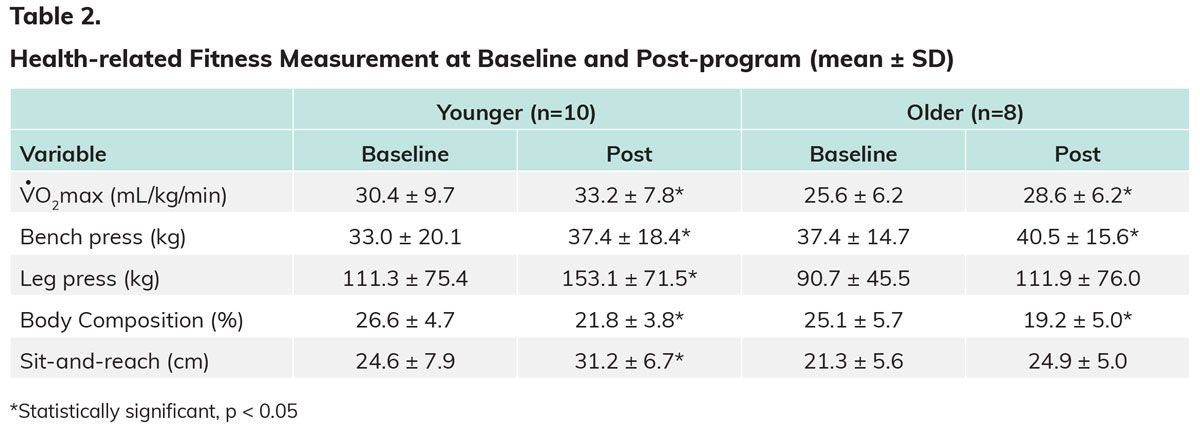
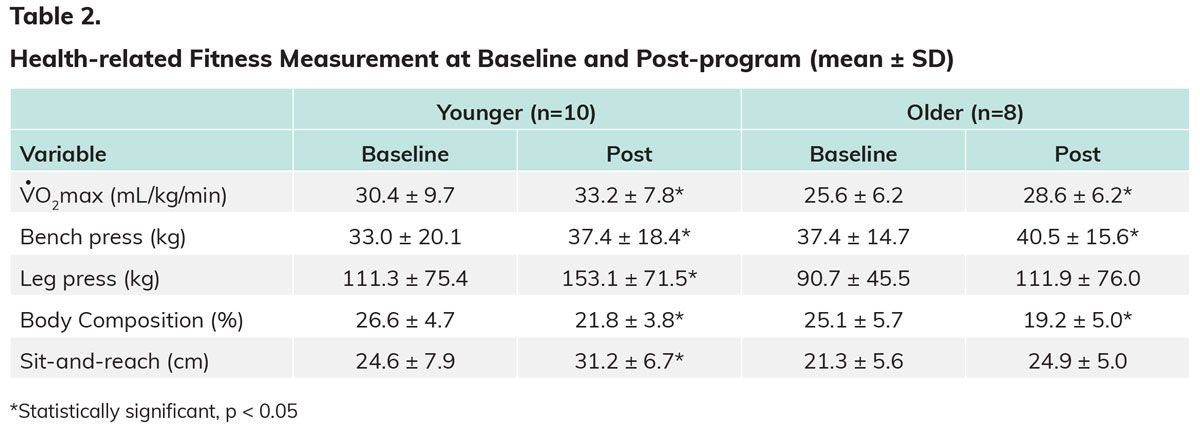
The health-related fitness measurements at baseline and post-program are presented in Table 2. As you can see, the younger group saw statistically significant changes in all variables, while the older group did not experience significant changes in either the leg press or sit-and-reach test. Importantly, there were no significant differences seen between younger and older participants when it came to changes in these health-related fitness measurements.
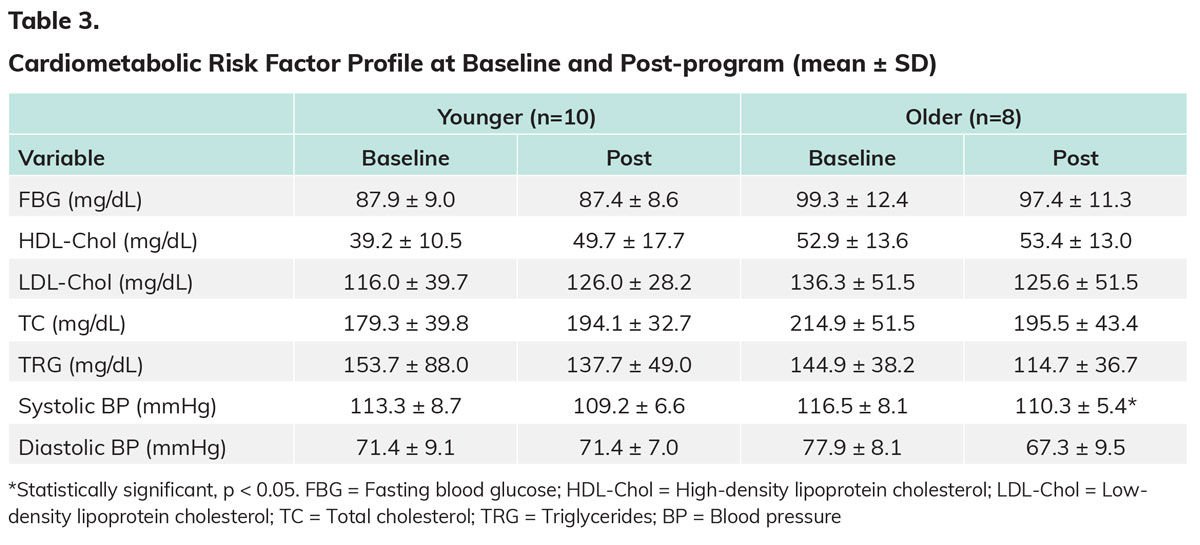
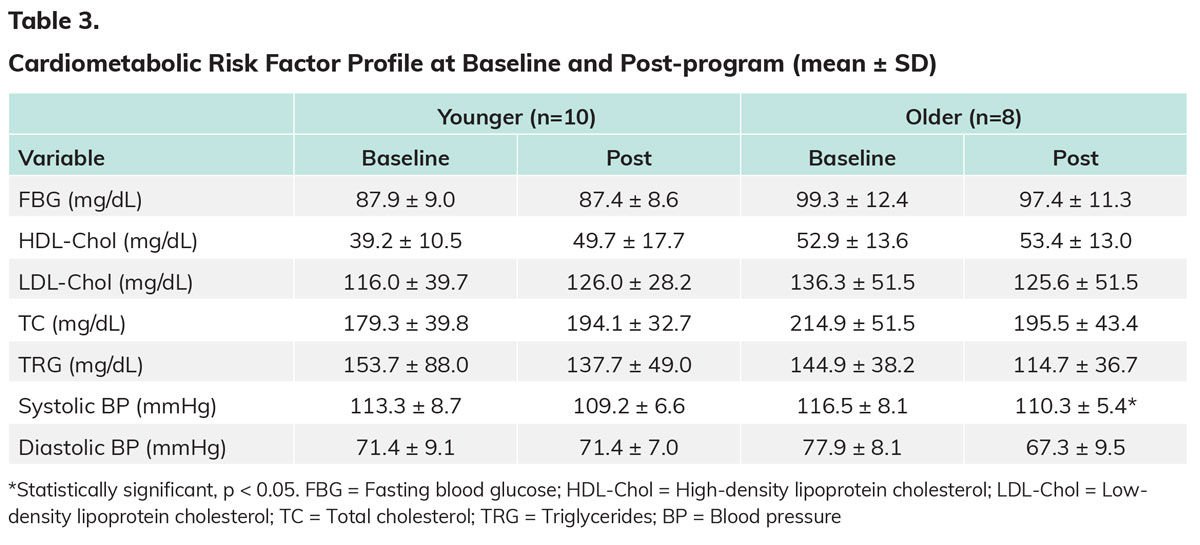
The cardiometabolic risk factor profiles at baseline and post-program are presented in Table 3. There were no statistically significant changes in any variable in the younger group, while the older group saw a significant decrease in systolic BP. When it came to cardiometabolic risk factor profiles, total cholesterol was improved more by older individuals compared to younger individuals. Otherwise, there were no differences between the two groups.
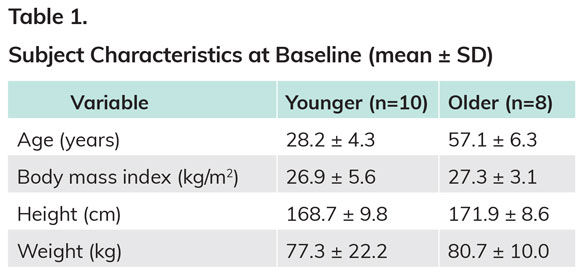
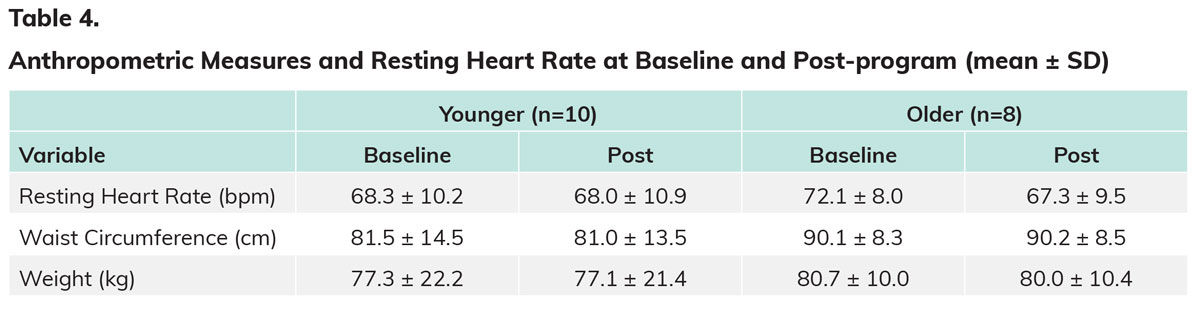
Finally, the anthropometric measures at baseline and post-program are presented in Table 4. There were no significant improvements for any variables in either group.
The Bottom Line
The primary finding of this study is that an individualized exercise program positively modified health-related fitness measurements to a similar extent in younger and older individuals. The personalized approach of the ACE IFT Model utilizes ventilatory threshold to program exercise, whereas other studies investigating age-related responses to exercise have used an estimated percent approach to program exercise intensity (i.e., percentage of maximal heart rate, VO2max or heart-rate reserve) (Weatherwax et al., 2018). Clearly, individualizing the exercise intensity and overall program is beneficial in eliciting the metabolic responses necessary to see favorable adaptations in measurements of health-related fitness (Dalleck et al., 2016; Wolpern et al., 2015).
So, to answer the question posed at the outset—do older adults respond to exercise training in a way that is similar to their younger counterparts?—the answer is a resounding “yes.” The older individuals in this study were able to adapt to personalized cardiorespiratory and functional/resistance training and improve health-related components of physical fitness to the same relative extent as the younger individuals. The one notable exception is that the older group had a harder time increasing lower-body strength to the same magnitude as the younger group. Dr. Dalleck explains that this may be due to the fact that the older cohort may have lost some type 2 muscle fibers simply as a result of aging, meaning that health coaches and exercise professionals may want to temper expectations when it comes to absolute strength gains seen in older adults.
What this research demonstrates is that clients are never too old to see statistically significant and meaningful gains as a result of a well-designed exercise program. “As long as we are not comparing a fit younger person to an older adult with cardiovascular disease or other chronic disease, for example,” explains Dr. Dalleck, “the older adult will experience similar gains when using the ACE IFT Model training paradigm.”
This ACE-sponsored study, “Do Younger and Older Adults Experience Similar Adaptations to Individualized Exercise Training?” was originally published in the peer-review Journal of Exercise Physiology Online.
References
American Council on Exercise (2014). ACE Personal Trainer Manual (5th ed.). San Diego: American Council on Exercise.
Dalleck, L.C. et al. (2016). Does a personalized exercise prescription enhance training efficacy and limit training unresponsiveness? A randomized controlled trial. Journal of Fitness Research, 5, 3.
Hoeger, W.W. et al. (2018). Lifetime of Physical Fitness and Wellness. Boston: Cengage Learning.
Karavidas, A. et al. (2010). Aging and the cardiovascular system. Hellenic Journal of Cardiology, 51, 5, 421-427.
Morley, J.E. et al. (2010). Nutritional recommendations for the management of sarcopenia. Journal of the American Medical Directors Association, 11, 6, 391-396.
Tuna, H.D. et al. (2009). Effect of age and physical activity level on functional fitness in older adults. European Review of Aging and Physical Activity, 6, 2, 99.
Weatherwax, R.M. et al. (2018). Using a site-specific technical error to establish training responsiveness: A preliminary explorative study. Open Access Journal of Sports Medicine, 9, 47.
Wolpern, A.E. et al. (2015). Is a threshold-based model a superior method to the relative percent concept for establishing individual exercise intensity? A randomized controlled trial. BMC Sports Science, Medicine and Rehabilitation, 7, 1, 16.





 by
by