Preparticipation health screening has long been a sticking point for personal trainers. Not only was the actual process complex, but knowing what to do with the information gathered could be confounding.
In the most recent edition of ACSM’s Guidelines for Exercise Testing and Prescription, the American College of Sports Medicine (ACSM, 2018) revamped its preparticipation health-screening recommendations. The result is a much more streamlined process that removes any unnecessary barriers to becoming more physically active, allows more clients to exercise without having to first visit their doctor and takes some of the decision-making burden away from the personal trainer.
The previous prescreening algorithms could result in excessive referrals to physicians for medical clearance, creating a potential barrier to adopting an exercise program. In addition, these referrals created a financial burden for both clients and the healthcare system.
The truth is, exercise is safe for most people and has many health and fitness benefits. When it comes to the cardiovascular risks associated with exercise, those risks decrease as individuals become more physically active and fit. In addition, exercise-related cardiovascular events are rare and are often preceded by warning signs and symptoms.
Stated simply, the last thing we want to do is unnecessarily discourage anyone from exercising.
The New Screening Process
The new process allows trainers to work immediately with more potential clients, creating the opportunity for a more rapid development of rapport and minimizing the risk of an individual leaving the fitness facility discouraged, never to return.
The new health-screening process is based on three factors that have been identified as important risk modulators of exercise-related cardiovascular events:
- The individual’s current level of physical activity
- Diagnosed cardiovascular, metabolic or renal disease and/or the presence of signs or symptoms of cardiovascular, metabolic or renal disease
- The desired exercise intensity
Chris Gagliardi is ACE’s Lead Study Coach and holds all four ACE certifications. He believes it’s important to highlight the fact that physical-activity levels are now taken into consideration. “In the past,” Gagliardi explains, “known cardiovascular or metabolic disease was an automatic red light from the trainer’s perspective. Now, if a client with known disease is symptom-free and a regular exerciser, he or she can work at a low-to-moderate exercise intensity without having to visit a doctor first.”
The removal of this barrier eliminates several steps that came before the client was even able to work out for the first time. Less back-and-forth with doctors means that clients can get started with their programs more easily and still feel safe doing so.
The new screening protocol also makes general recommendations for medical clearance, leaving the specifics—such as the need for medical exams or exercise tests—up to the discretion of the healthcare provider.
The previous risk-classification process included recommendations like “medical exam recommended before exercise” and “doctor supervision of exercise test.”
“Now, those decisions are left up to the physicians,” says Gagliardi. “All that is required of the personal trainer is making the referral when appropriate and securing any needed medical clearance.”
The goal of this process is to identify individuals:
- Who should receive medical clearance before initiating an exercise program or increasing the frequency, intensity and/or volume of their current program
- With clinically significant disease(s) who may benefit from participating in a medically supervised exercise program
- With medical conditions that may require exclusion from exercise programs until those conditions are abated or better controlled
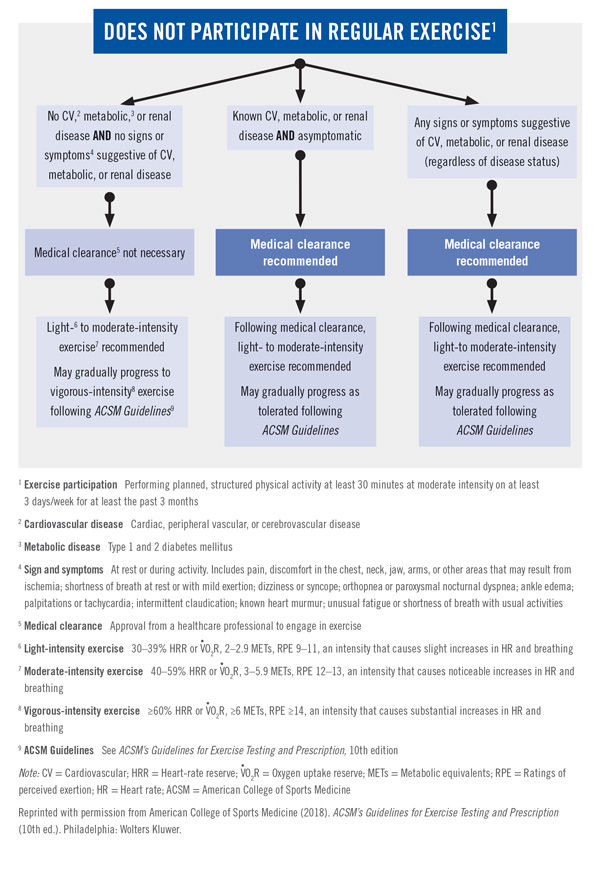
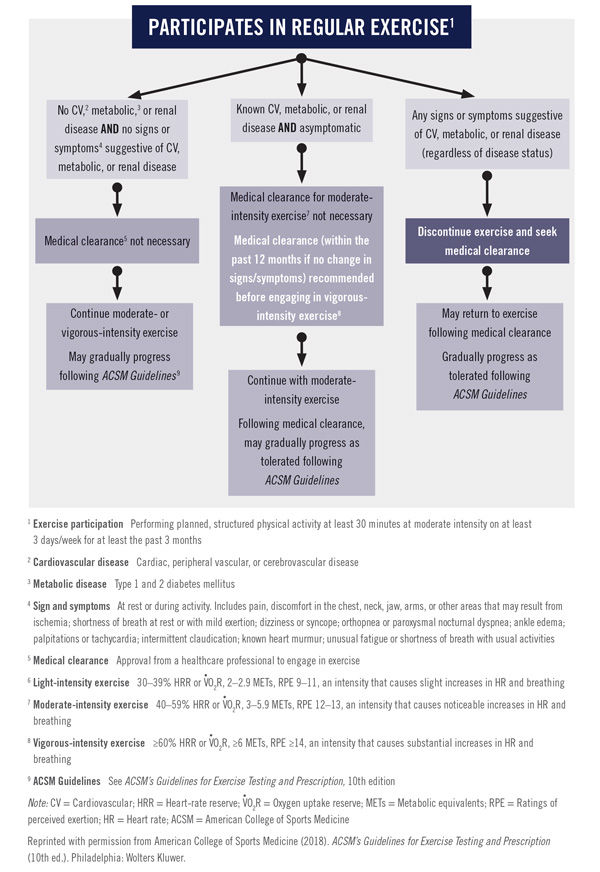
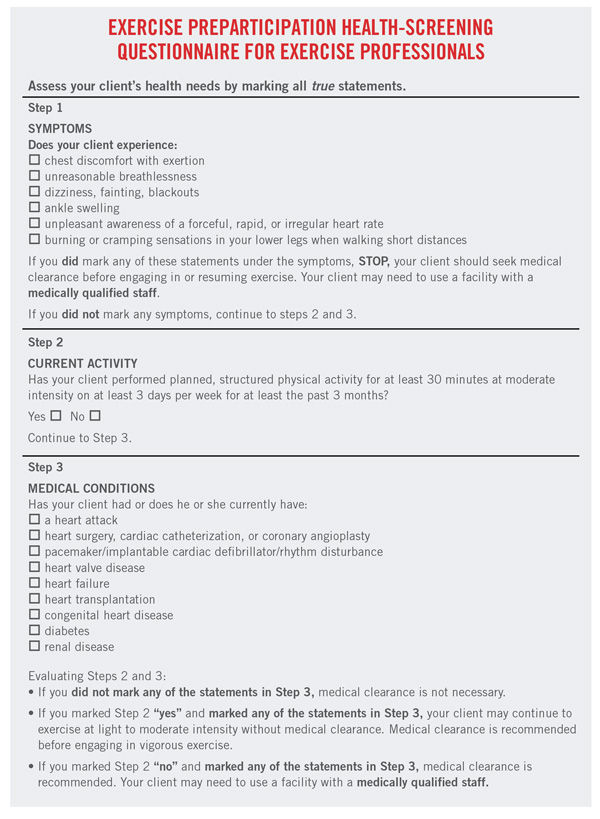
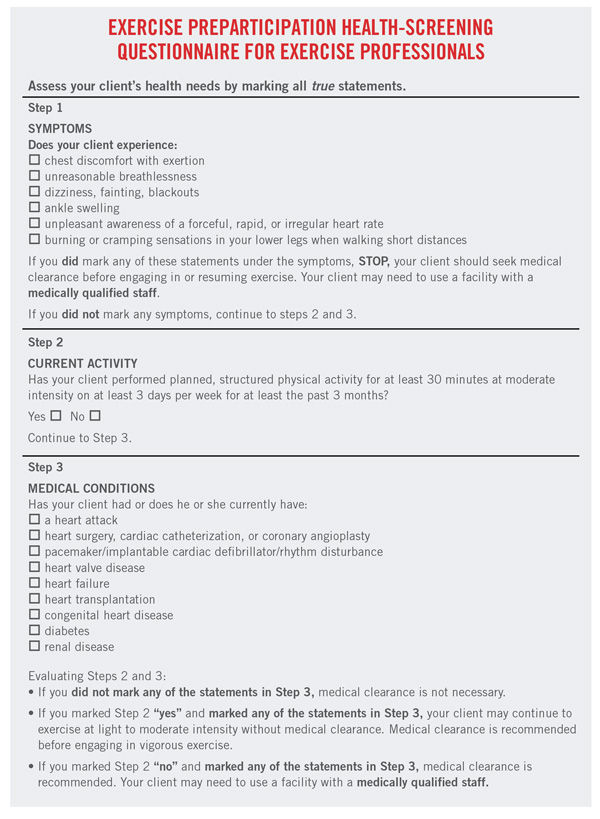
Figure 1 presents the preparticipation health-screening algorithm, while an exercise preparticipation checklist is presented in Figure 2. This algorithm shows that medical clearance is needed only under the following circumstances:
- For those who do not exercise regularly: If a client has cardiovascular, metabolic or renal disease, or signs or symptoms that suggest he or she does, then medical clearance is necessary.
- For regular exercisers: If a client has signs or symptoms suggestive of cardiovascular, metabolic or renal disease, he or she should discontinue exercise and seek medical clearance. If a client has a known history of cardiovascular, metabolic or renal disease and has a desire to progress to vigorous-intensity aerobic exercise, medical clearance is recommended.
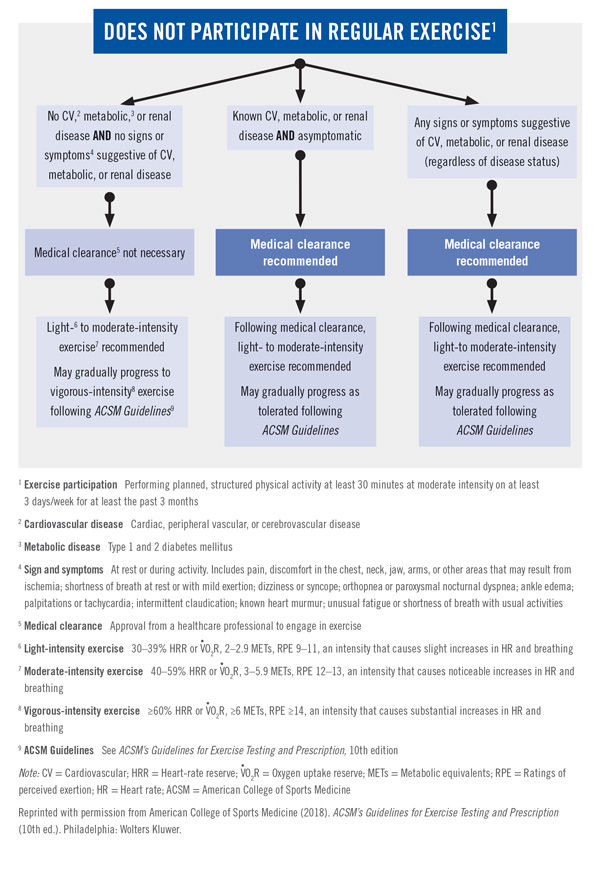
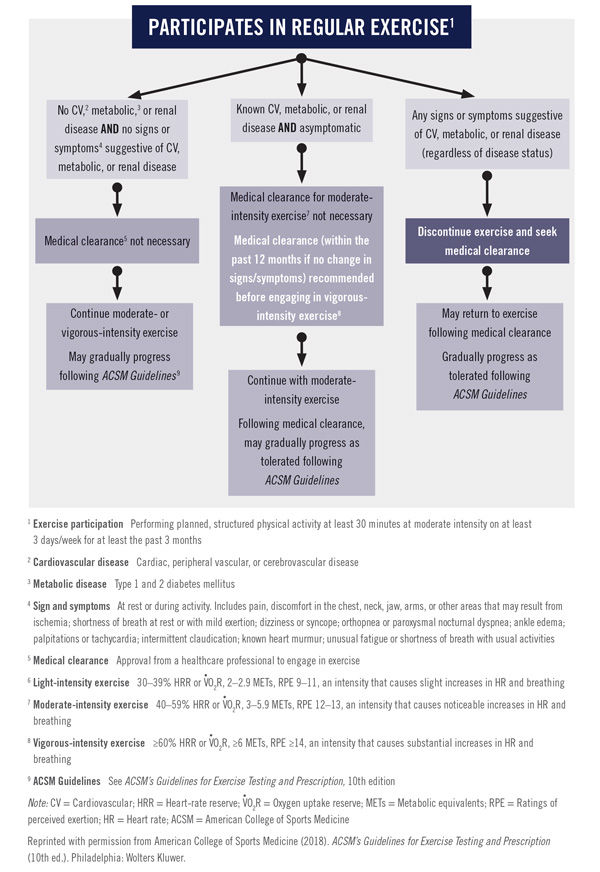
While the identification of the signs and symptoms referenced in this algorithm may be within the scope of practice of most health and fitness professionals, interpretation of those same signs and symptoms should be made only by qualified, licensed professionals within the context in which they appear (ACSM, 2018):
- Pain; discomfort (or other angina equivalent) in the chest, neck, jaw, arms or other areas that may result from myocardial ischemia
- Shortness of breath at rest or with mild exertion (dyspnea)
- Dizziness or syncope, most commonly caused by reduced perfusion to the brain
- Orthopnea (dyspnea in a reclined position) or paroxysmal nocturnal dyspnea (onset is usually two to five hours after the beginning of sleep)
- Ankle edema
- Palpitations or tachycardia
- Intermittent claudication (pain sensations or cramping in the lower extremities associated with inadequate blood supply)
- Known heart murmur
- Unusual fatigue or shortness of breath with usual activities
Resistance Training
Current evidence is insufficient regarding cardiovascular complications during resistance training to warrant formal prescreening recommendations (ACSM, 2018). Little data are available on the topic, but it appears that the risk of complications is low.
Self-guided Screening
Preparticipation health screening for individuals wanting to initiate an exercise program should be conducted using the 2017 Physical Activity Readiness Questionnaire for Everyone (PAR-Q+) form.
This form is evidence-based and was developed with a goal of reducing unnecessary barriers to exercise. The PAR-Q+ can be used as either a self-guided screening tool or as an additional element of screening for health and fitness professionals seeking additional client information.
Patients in Cardiac Rehabilitation and Medical Fitness Facilities
Health and fitness professionals working with clients with known cardiovascular disease in clinical settings, such as cardiac rehabilitation and medical fitness facilities, should use a more in-depth screening tool than the one just presented (ACSM, 2018). Specifically, it is recommended they use risk-stratification criteria from the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR).
Identifying Risk Factors Is Still Important
A main feature of the previous screening protocol was the identification of each client’s cardiovascular disease risk-factor threshold, which was then used as the basis for the classification of his or her risk and the plan going forward. For example, a woman who had a sedentary lifestyle, stage 1 hypertension and a body mass index (BMI) of 32 kg/m2 would have a total score of 3, placing her in either the moderate- or high-risk category, depending on the presence of symptoms of disease.
Gagliardi says that, while risk classification is no longer part of the screening process, this is still important information to gather in the early stages of any client–trainer relationship. “Understanding a client’s medical history is essential, as it allows for the individualization of both the programming and education for that client moving forward,” he says. In addition, Gagliardi points out that this data can serve as a baseline for any exercise programming or lifestyle change. Imagine being able to show the aforementioned client that by establishing and then maintaining an exercise routine that reduced her blood pressure and lowered her BMI to below the obesity threshold, she would have eliminated three risk factors for cardiovascular disease.
In Conclusion
When using the previous health-risk screening protocol, personal trainers were often left frustrated because of the number of referrals required. In fact, the vast majority of clients had to go to the doctor before they could begin working with the trainer, and many of them would never make it back to the gym. The new screening process is much more user-friendly and allows personal trainers to work with more individuals more quickly.
Reference
American College of Sports Medicine (2018). ACSM’s Guidelines for Exercise Testing and Prescription (10th ed.). Philadelphia: Wolters Kluwer.





 by
by