Darius is a physically active 40-something attorney who enjoys strength-training workouts along with playing both pick-up basketball and golf. Richard is a 30-something retail manager whose regular exercise routine includes resistance training, high-intensity interval training and playing basketball at every opportunity. Besides their love of basketball, these two men, along with thousands of other men in their age bracket, have something else in common: They have experienced significant injuries in the lower-leg muscles. During a basketball game at his health club, Darius suffered a complete rupture of his Achilles tendon, which took almost a full year to heal. Richard tore the peroneus brevis muscle in the bottom of his foot, which resulted in having to wear a boot for two months along with a lengthy rehabilitation.
Common Injuries of the Lower Leg and Foot
An estimated 75 percent of American adults will experience foot pain at some point in their lives. It is also estimated that in a population of 100,000 adults, at least 18 individuals will experience significant injuries, such as a rupture or tear to the Achilles tendon; most of those injuries (68 percent) occur during participation in a sport or recreational activity. A majority of individuals who experience a significant injury to the Achilles tendon are athletically active men between the ages of 30 and 55. Of all sports-related Achilles injuries, approximately half (47 percent) were related to basketball; approximately 20 percent of Achilles injuries were related to daily activities including walking or carrying objects (Raikin, 2014).
The lower leg and foot are a complex structure of muscles, tendons, ligaments and bones responsible for withstanding significant stresses during upright activities like walking, running or jumping. The lower leg and foot are the interface between the body and the ground. Every time the foot makes contact with the ground it has to mitigate the forces caused by gravity accelerating the weight of an individual’s body downward, as well as the upward impulse of force created by the solid ground. As a result of the tremendous magnitude created by these two competing forces, recreationally active adults, like Darius and Richard, are at risk of experiencing injuries to the muscles of the foot and lower leg; specifically, muscle damage on the bottom of the foot (including plantar fasciitis) and to the Achilles tendon.
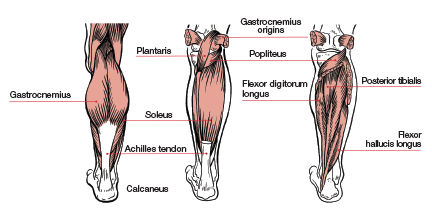
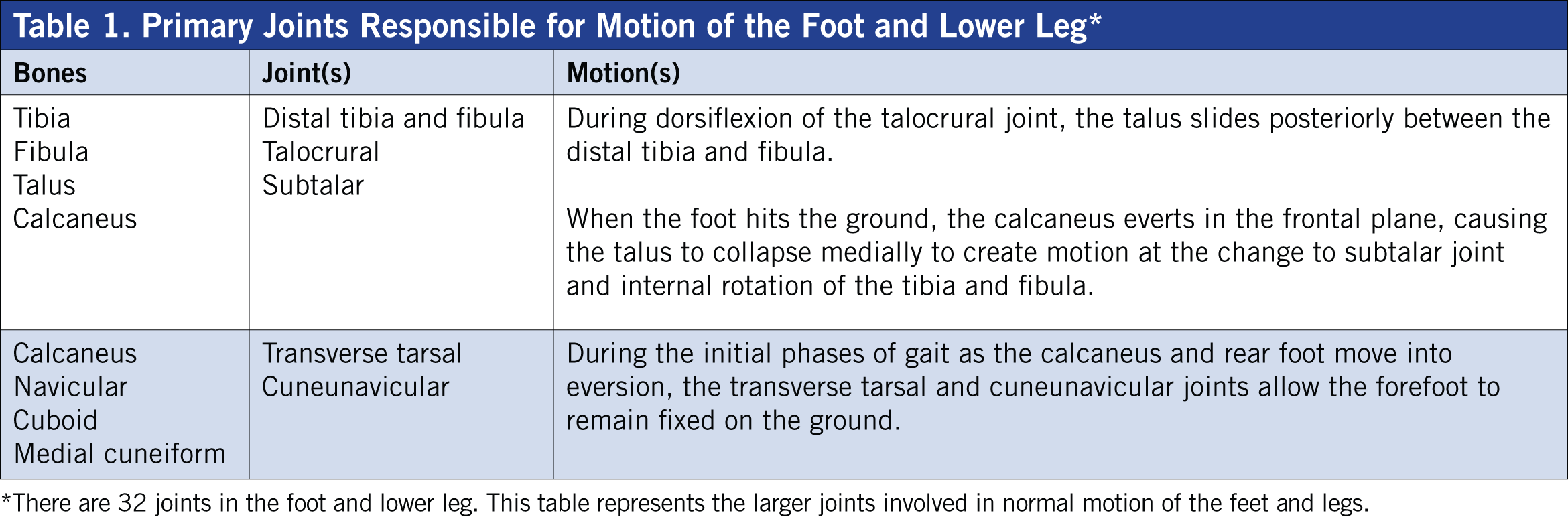
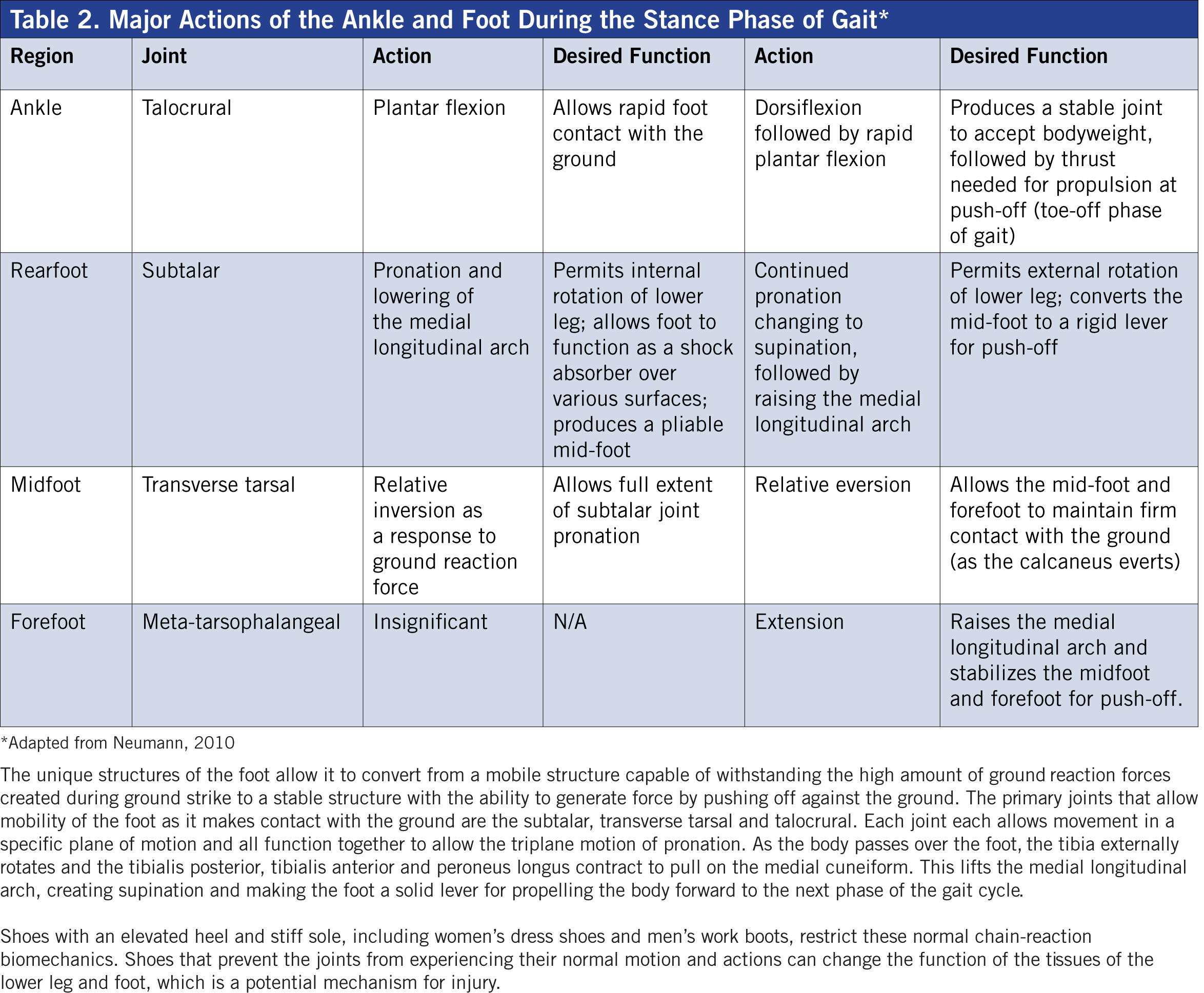
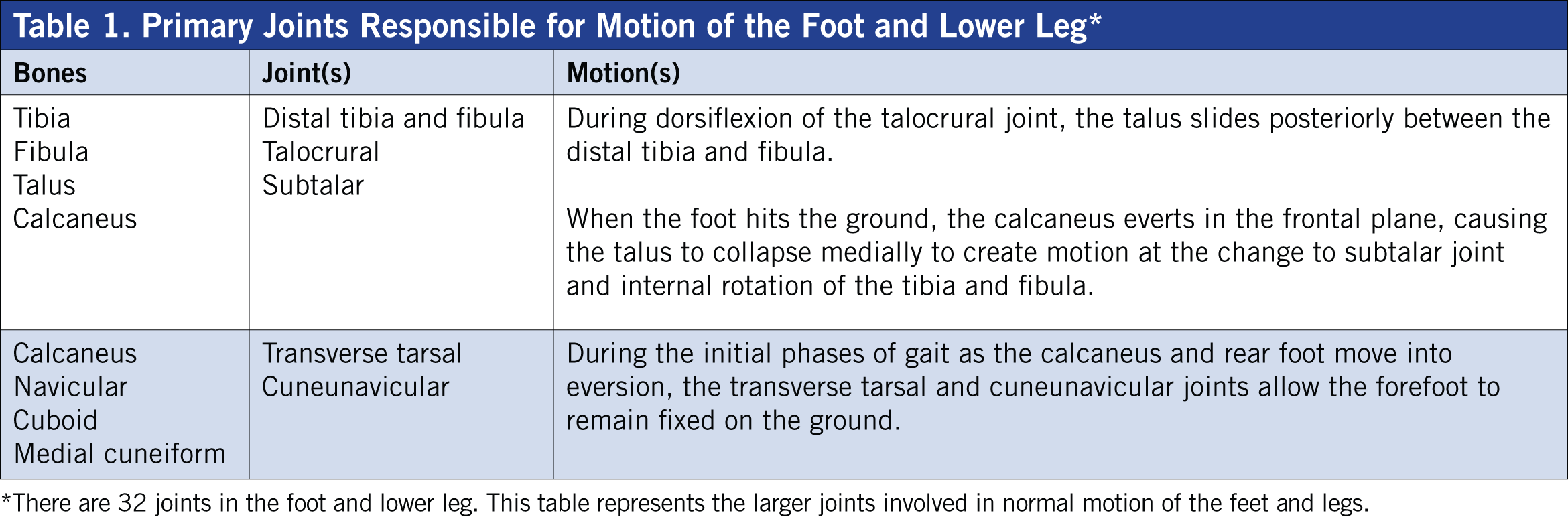
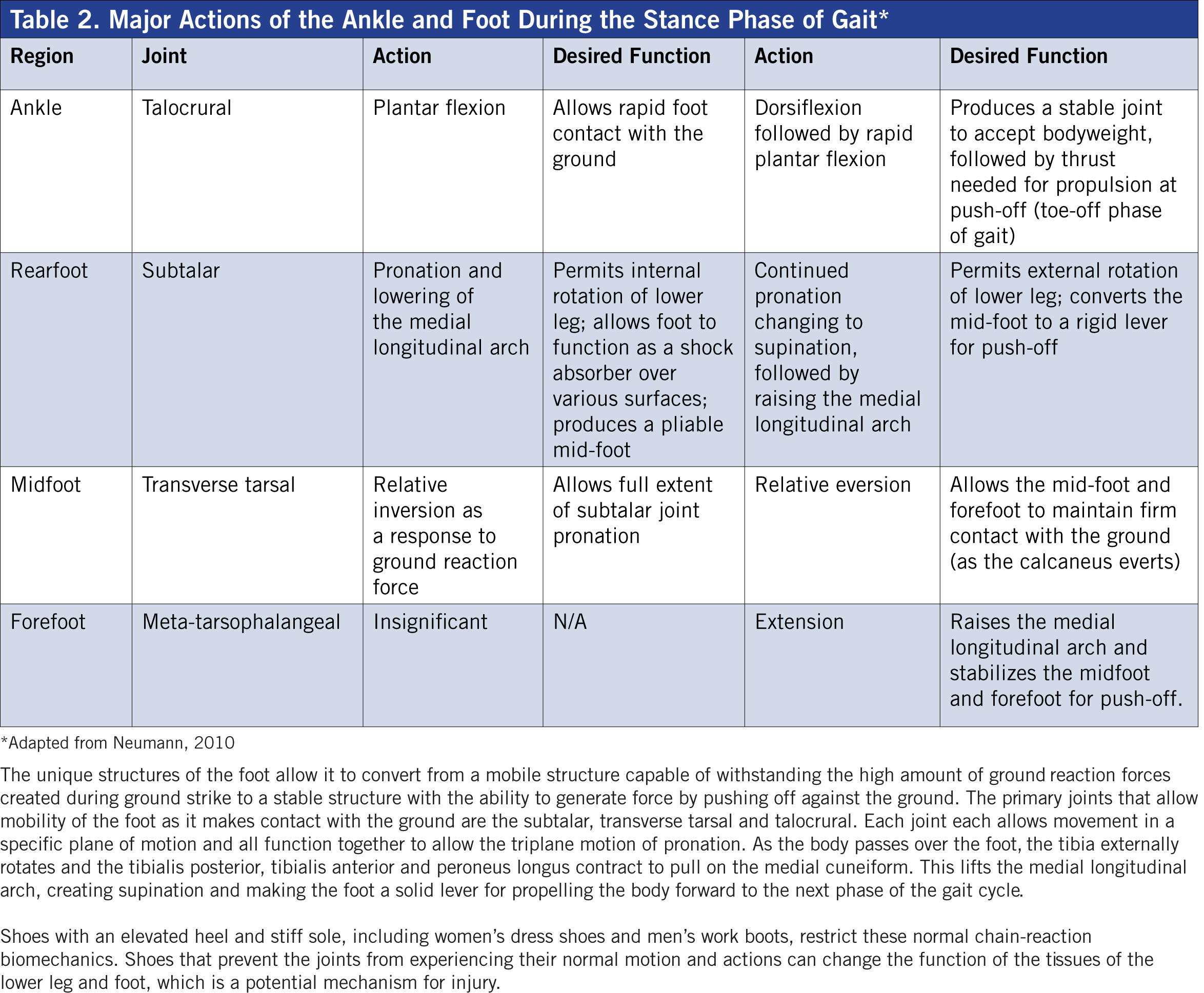
The foot and lower leg must have the mobility to facilitate a variety of forces and surfaces, yet provide the stability to push against the ground during walking and running. The human ankle and foot contain 28 muscles to control stability and mobility at 32 joints, which are organized into three specific regions: rearfoot, midfoot and forefoot (Tables 1 and 2). According to physical therapist and founder of the Gray Institute, Gary Gray, “[Personal trainers] need to understand the role that the lower leg muscles play during gait, specifically how the foot functions when it makes contact with the ground and reacts as the body is passing over it.”
While it is outside your scope of practice as a health and fitness professional to diagnose an injury, it is completely appropriate to understand the mechanisms of common injuries to be able to design exercise programs that can help clients reduce the risk of becoming injured or help them return to their favorite activities after the appropriate medical intervention. Understanding how the foot and lower leg function together during upright movement is essential to designing exercise programs that can improve the strength and resiliency of these muscles and help clients avoid debilitating injuries that can keep them from their favorite activities.
Biomechanics of the Lower Leg and Foot
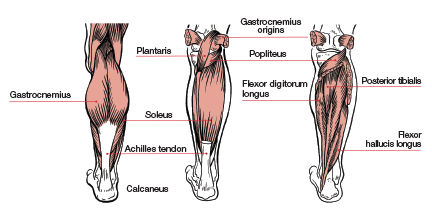
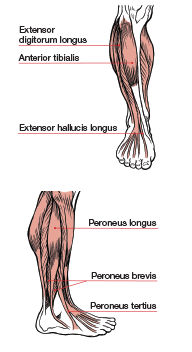 The traditional understanding of the lower leg, specifically the gastrocnemius and soleus muscles of the calf, suggests that they work most effectively to create plantar flexion. Toe raises, both with and without resistance, are often recommended as an effective exercise for strengthening these muscles. However, these exercises could be a potential cause of common lower-leg and foot injuries. Yes, the calves can point the toes, but during integrated movements, such as walking or running, they are responsible for controlling motion of the foot as well as supporting mobility of the hip. When it comes to how the muscles of the lower leg function during upright activities such as walking, running and jumping, it is important to know how all of the muscles and joints work together to create successful movement (Table 3). Instead of helping to improve performance, strength-training programs that focus on just one or two muscles of the lower leg could be setting individuals up for injury.
The traditional understanding of the lower leg, specifically the gastrocnemius and soleus muscles of the calf, suggests that they work most effectively to create plantar flexion. Toe raises, both with and without resistance, are often recommended as an effective exercise for strengthening these muscles. However, these exercises could be a potential cause of common lower-leg and foot injuries. Yes, the calves can point the toes, but during integrated movements, such as walking or running, they are responsible for controlling motion of the foot as well as supporting mobility of the hip. When it comes to how the muscles of the lower leg function during upright activities such as walking, running and jumping, it is important to know how all of the muscles and joints work together to create successful movement (Table 3). Instead of helping to improve performance, strength-training programs that focus on just one or two muscles of the lower leg could be setting individuals up for injury.
This installment of ACE’s functional anatomy series examines how the muscles of the lower leg are designed to function as an integrated unit to help the foot convert from a mobile structure when it hits the ground during the ground-contact phase of gait to a stable lever capable of pushing off of the ground to propel the body forward.
Muscle contains two primary types of tissue: (1) the inelastic contractile element of actin and myosin responsible for creating a shortening force and the elastic component of connective tissue, and (2) fascia that is interwoven between every individual muscle fiber (Schleip, 2012). The contractile element initiates the forces required to move bones, while the elastic tissue lengthens in response to applied forces. The muscles of the lower leg are an excellent example of how these two properties of tissue must work effectively to create efficient, injury-free movement.
How a muscle functions as it lengthens can, in fact, be more important than how it is designed to function during the concentric, shortening phase of muscle action. The most effective way to learn how the structures of the lower leg and foot function is to identify what they do during the gait cycle of walking or running (see Table 2). At the initial, ground-contact phase of gait, the foot experiences the triplane motion of pronation, which is a combination of the talocrural joint plantar flexing in the sagittal plane and the calcaneus rolling into eversion in the frontal plane, while the tibia experiences internal rotation in the transverse plane (Neumann, 2010).
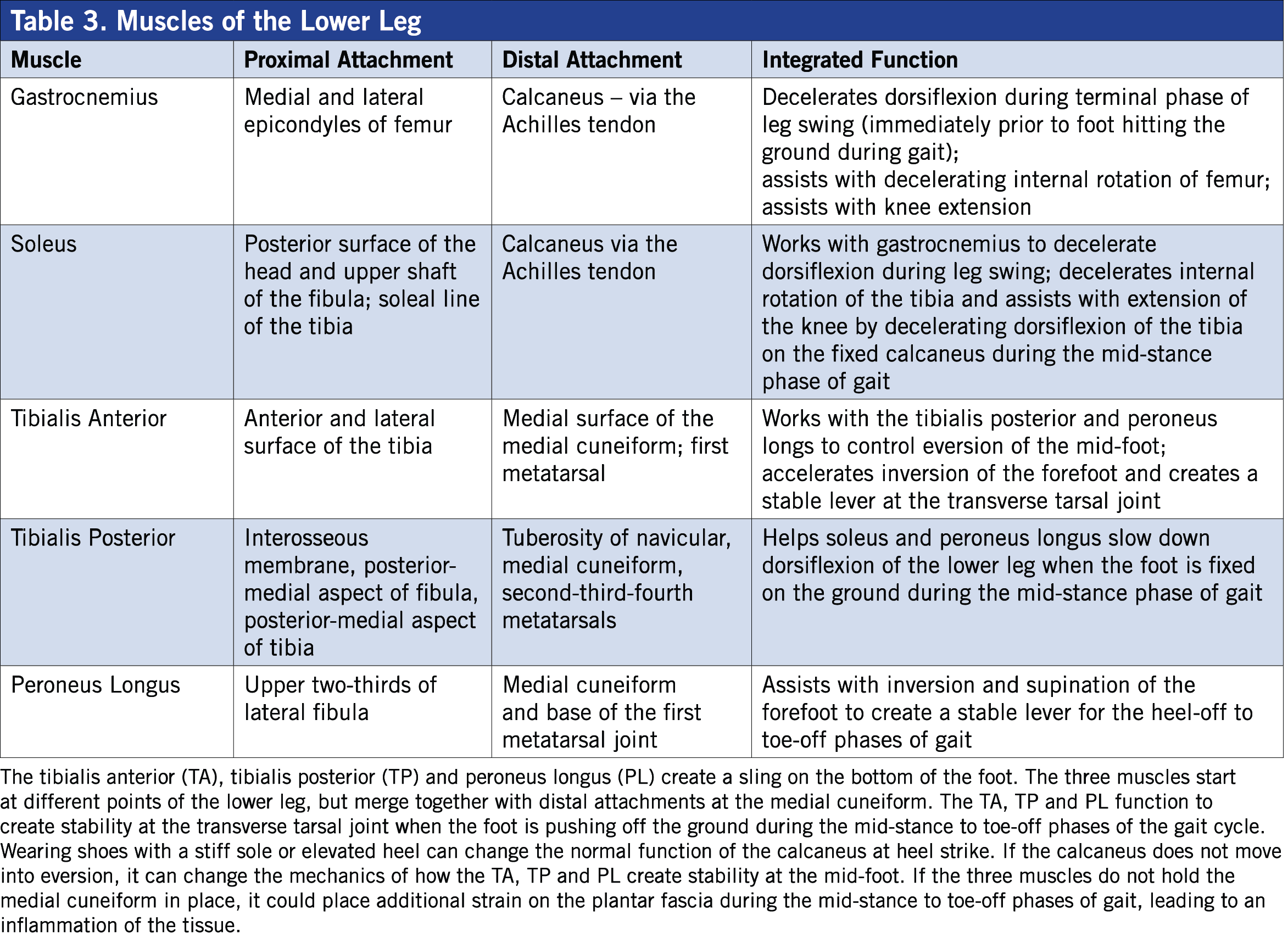
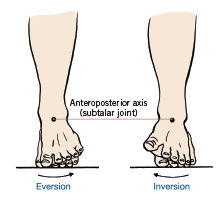 Pronation is a normal motion designed to allow the foot to absorb the weight of the body. During pronation as the foot and lower leg hit the ground, the muscles responsible for dorsiflexing and supinating the foot lengthen eccentrically to decelerate the forces created by gravity and ground reaction. An important shock-absorption mechanism is the medial longitudinal arch, which depresses during the ground-contact and early midstance phases of gait. As the body passes over the foot in midstance, the motion of the foot changes from pronation to supination as the same muscles responsible for decelerating pronation suddenly shorten to lift the medial longitudinal arch to create supination. Pronation allows the foot to be mobile to absorb ground forces. Supination occurs during the later phases of gait, causing the foot to be a solid lever for pushing off against the ground. During the mid-to-later phases of gait, when the foot is changing from pronation to supination, the entire leg changes direction from flexing, adducting and internally rotating to extending, abducting and externally rotating (Neumann, 2010; Gray and Tiberio, 2007). During this normal chain reaction of biomechanics, several muscles in the foot and leg must work together to both absorb and generate force. If the tissues of the foot lose the extensibility and strength to control these forces, it could result in a number of injuries, including plantar fasciitis and Achilles tendon ruptures (Gray and Tiberio, 2007).
Pronation is a normal motion designed to allow the foot to absorb the weight of the body. During pronation as the foot and lower leg hit the ground, the muscles responsible for dorsiflexing and supinating the foot lengthen eccentrically to decelerate the forces created by gravity and ground reaction. An important shock-absorption mechanism is the medial longitudinal arch, which depresses during the ground-contact and early midstance phases of gait. As the body passes over the foot in midstance, the motion of the foot changes from pronation to supination as the same muscles responsible for decelerating pronation suddenly shorten to lift the medial longitudinal arch to create supination. Pronation allows the foot to be mobile to absorb ground forces. Supination occurs during the later phases of gait, causing the foot to be a solid lever for pushing off against the ground. During the mid-to-later phases of gait, when the foot is changing from pronation to supination, the entire leg changes direction from flexing, adducting and internally rotating to extending, abducting and externally rotating (Neumann, 2010; Gray and Tiberio, 2007). During this normal chain reaction of biomechanics, several muscles in the foot and leg must work together to both absorb and generate force. If the tissues of the foot lose the extensibility and strength to control these forces, it could result in a number of injuries, including plantar fasciitis and Achilles tendon ruptures (Gray and Tiberio, 2007).
The Achilles Tendon
The Achilles tendon is formed by the gastrocnemius and soleus muscles of the lower leg and attaches to the heel of the foot at the calcanea tuberosity. Injuries to the Achilles are common in middle-aged “weekend warriors” who don’t participate in an appropriate exercise program or take the time to warm up properly before participating in their favorite activities. Factors that increase the risk of an Achilles tendon injury include age, body weight and activity. Older and heavier individuals have a higher risk of injury. Participating in activities that require explosive movements like jumping, landing or making rapid changes of direction, all of which are common during basketball, also increases risk (Wertz, Galli and Borchers, 2013).
As experienced by Darius, a rupture or tear to the Achilles tendon can be extremely painful, and recovery and rehabilitation can last up to a full calendar year. It’s important to note that most Achilles injuries happen during the spring and summer months, with significantly fewer happening during the winter (Raikin, 2014). What does this mean for health and fitness professionals? If you work with clients who you know will be playing sports such as basketball, tennis or soccer, you can help reduce their risk of experiencing a debilitating Achilles injury by implementing a proper exercise and conditioning program.
The Achilles tendon is the largest and strongest tendon in the human body, capable of withstanding loads up to 10 times of an individual’s body weight during dynamic activities such as sprinting or jumping. It is hypothesized that a loss of elasticity resulting in muscle-tendon stiffness is a common cause of injury (Raikin, 2014). The third law of physics states that for every action there is an equal and opposite reaction. When your foot hits the ground, the downward force of your body weight is transmitted into the ground. At the same time, that ground-reaction force is being transmitted back up into your body. As you quickly transition from the ground-strike to midstance phases of gait, the Achilles tendon experiences a rapid lengthening force, which is increased significantly during high-speed activities such as jumping or sprinting. The muscles of the lower leg and foot need to be extensible in all three planes of motion to allow proper joint motion to occur during normal upright movements. For very active individuals, however, the tissues of the lower leg and foot need to be specifically conditioned to withstand the high forces produced by rapid changes of direction, jumping or landing. One reason why Achilles tendon injuries may be common among older athletic individuals such as Darius and Richard is that over the course of the natural aging process, the elastic connective tissue of fascia and tendons can lose their elasticity (Schleip, 2012).
When combined with exercises such as calf raises that focus on the concentric properties of contractile tissue, this natural loss of elasticity presents an instantly recognizable mechanism for lower-leg injuries. Calf raises can enhance strength and stiffness of the contractile element in lower-leg muscles, but will not improve the elasticity of the connective tissue of the Achilles tendon or fascia at the plantar surface (bottom) of the foot. An exercise program that focuses solely on the concentric action of plantar flexion during calf raises will not adequately prepare lower-leg and foot muscles for the rapid lengthening and high eccentric loads they will experience when landing or making rapid changes of direction. “We find that exercises that do not reinforce what happens during normal function are not effective at improving the performance of the muscle,” explains Gray, “or the part of the body that muscle is supposed to control.”
The Soleus Can Extend the Knee
A muscle does not always need to cross a joint to affect motion at the joint. For example, the soleus muscle of the lower leg attaches on the tibia so it does not cross the knee, yet it can influence motion at the knee. During the midstance to early heel-off phases of gait, the tibia is dorsiflexing over a relatively fixed calcaneus. As that happens, the soleus is lengthened, which restricts forward motion of the tibia. As the tibia stops moving forward over the fixed calcaneus, the opposite leg is swinging forward. As this is happening, the knee above the foot in midstance is moving into extension. Because the soleus restricts this forward motion of the tibia, it aids in extending the knee during gait.
Exercises such as multiplanar lunges that keep the foot fixed on the ground while the rest of the body moves can improve the extensibility of the soleus, anterior tibialis and posterior tibialis, helping them to become more efficient at converting from lengthening to shortening, which is how they function during the normal gait cycle (Gray and Tiberio, 2007).
The Calf as a Core Muscle
Movement of the foot and lower leg have a direct impact on motion of the proximal portion of the femur as it inserts into the iliofemoral (hip) joint of the pelvis. Internal rotation of the tibia creates internal rotation at the iliofemoral joint of the hip. If the calf muscles become overly tight, it can change the motion of both the lower leg and hip joints. This can, in turn, change the length-tension relationships and function of the muscles responsible for controlling motion at the hip.
The superior attachments of the gastrocnemius attach at the medial and lateral condyles on the distal end of the femur. At the proximal femur the greater trochanter inserts into the pelvis at the acetabulum. Tightness in the calf muscles can change the range of motion of the hip. If the hip loses range of motion, it can change the position of the pelvis and lumbar spine, which will affect the muscles commonly referred to as the core. “During gait the heel raises off of the ground as a reaction to what the hip flexors do, which is to restrict extension of femur in the sagittal plane,” explains Gray, “and not as the result of contraction of the plantar flexors.”
Understanding how all muscles work together to create coordinated movement is an important component of being a successful health and fitness professional.
The unique structures of the foot allow it to convert from a mobile structure capable of withstanding the high amount of ground reaction forces created during ground strike to a stable structure with the ability to generate force by pushing off against the ground. The primary joints that allow mobility of the foot as it makes contact with the ground are the subtalar, transverse tarsal and talocrural. Each joint each allows movement in a specific plane of motion and all function together to allow the triplane motion of pronation. As the body passes over the foot, the tibia externally rotates and the tibialis posterior, tibialis anterior and peroneus longus contract to pull on the medial cuneiform. This lifts the medial longitudinal arch, creating supination and making the foot a solid lever for propelling the body forward to the next phase of the gait cycle.
Shoes with an elevated heel and stiff sole, including women’s dress shoes and men’s work boots, restrict these normal chain-reaction biomechanics. Shoes that prevent the joints from experiencing their normal motion and actions can change the function of the tissues of the lower leg and foot, which is a potential mechanism for injury.
Strength Training for the Lower Leg and Foot
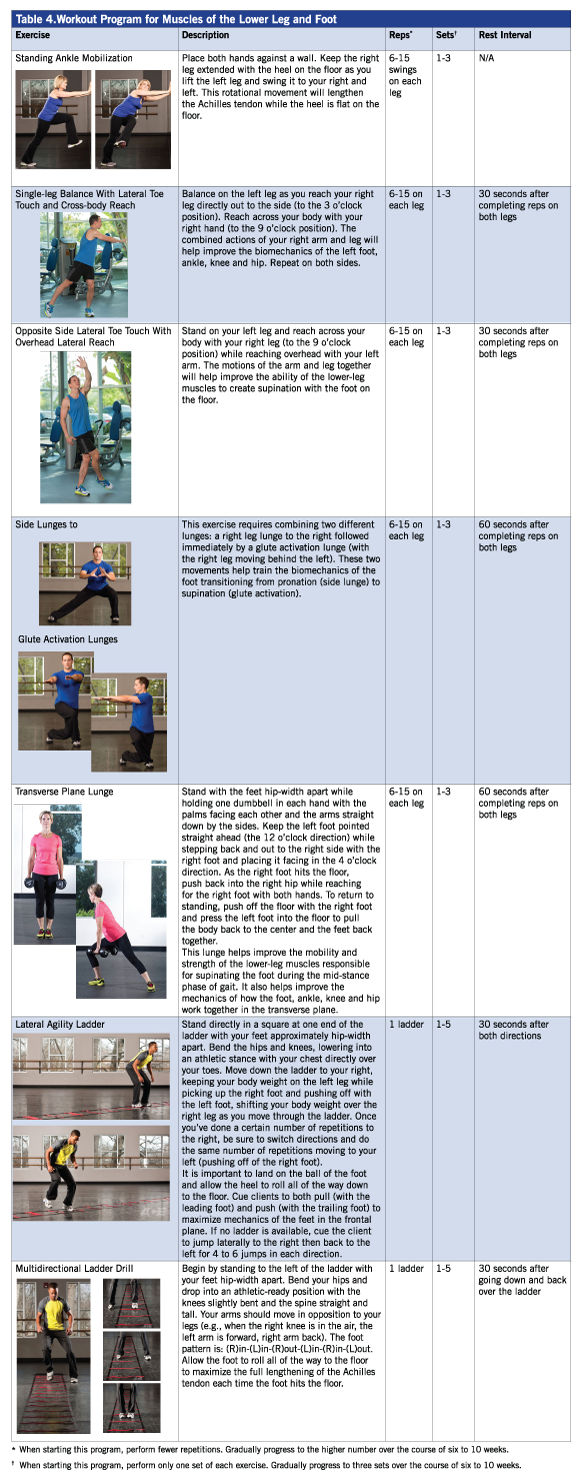
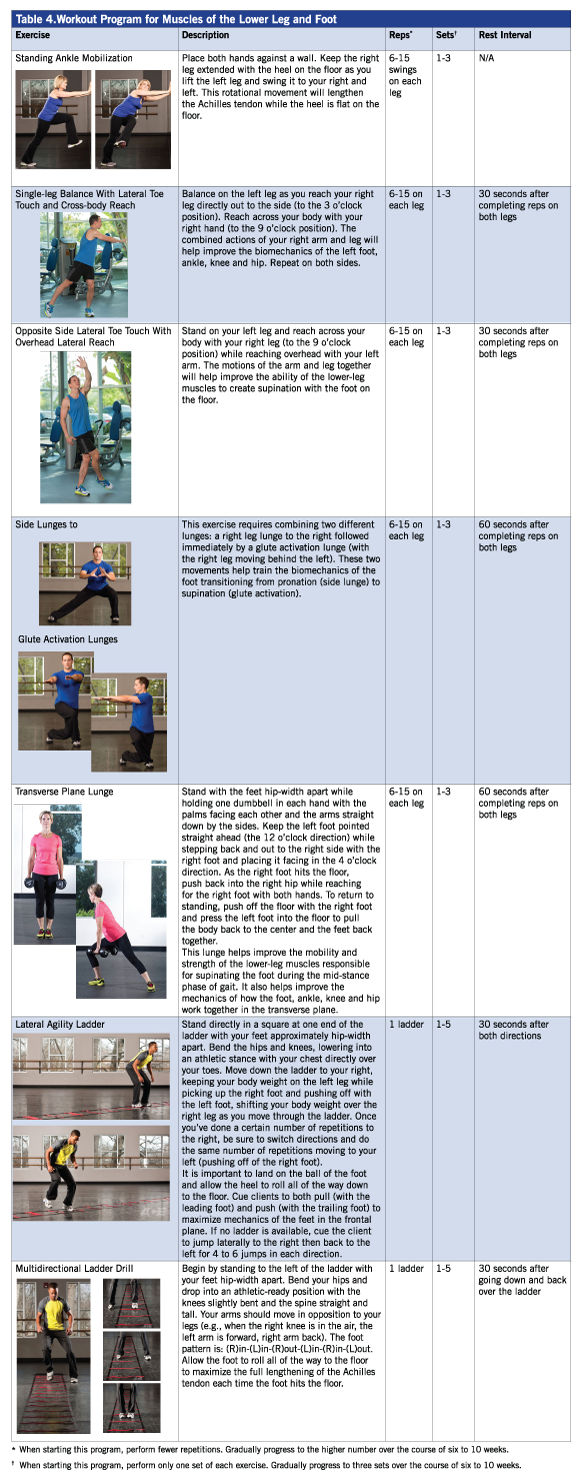
Proper strength training for the muscles of the lower leg should focus on helping the normal biomechanics that allow the foot to convert from mobility to stability, as well as increasing the elasticity of the fascia and connective tissue. It is also important to use exercises that involve the whole leg to improve how all of the joints, from the transverse tarsal in the midfoot to the iliofemoral of the hip, function together during upright movements.
For example, proper hip extension relies on the ability of the tibia to dorsiflex over the foot when it is fixed on the ground during the midstance phase of gait. The only way to improve this function is to use movements that involve all of the leg joints together. Standing on one leg and moving the body in all planes of motion using toe touches, lunges and bounds (leaping from one foot to the other) can be extremely effective for strength training and injury prevention.
When introducing dynamic lower-leg exercises to clients (Table 4), start with a limited number of reps and sets to allow the soft tissues of the fascia and elastic connective tissue to adapt to the rapid lengthening before progressing to the high volumes required for optimal performance enhancement. In normal, asymptomatic tissue, it should take about six to 10 weeks to progress from single sets of four to eight repetitions to multiple sets of 10 to 15 repetitions (on each leg).
Conclusion
When told about the need to train the elastic component of soft tissue, Darius immediately recognized his mechanism of injury. Apparently, he had been wearing stiff-soled dress shoes and, upon arriving at the gym, immediately hopped right into a basketball game without taking the time to properly warm up. Since returning to his normal exercise routine, Darius has made mobility training a key component of his workout programs and credits it with enabling him to enjoy his favorite activities. Before he hops on the court or plays a round of golf, Darius makes sure he performs a variety of movement patterns in all three planes of motion to ensure he is ready to begin. The good news is that having this understanding of how the lower leg and foot function can help you to make sure your clients and group fitness participants avoid a debilitating injury and remain engaged in their favorite activities.
References
Gray, G. and Tiberio, D. (2007). Gray Institute of Functional Transformation (48-week education course).
Neumann, D. (2010). Kinesiology of the Musculoskeletal System: Foundations for Rehabilitation (2nd ed.). St. Louis, Mo.: Elsevier.
Raikin, S. (2014). Epidemiology of Achilles tendon rupture in the U.S.: Lower extremity review.
Schleip, R. et al. (2012). Fascia: The Tensional Network of the Human Body. London: Churchill Livingstone.
Wertz, J., Galli, M. and Borchers, J. (2013). Achilles tendon rupture for aerial and ground athletes. Sports Health, 5, 5, 407-409.





 by
by 

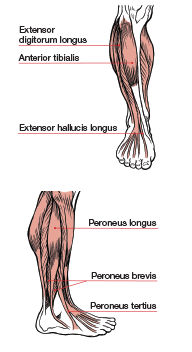 The traditional understanding of the lower leg, specifically the gastrocnemius and soleus muscles of the calf, suggests that they work most effectively to create plantar flexion. Toe raises, both with and without resistance, are often recommended as an effective exercise for strengthening these muscles. However, these exercises could be a potential cause of common lower-leg and foot injuries. Yes, the calves can point the toes, but during integrated movements, such as walking or running, they are responsible for controlling motion of the foot as well as supporting mobility of the hip. When it comes to how the muscles of the lower leg function during upright activities such as walking, running and jumping, it is important to know how all of the muscles and joints work together to create successful movement (Table 3). Instead of helping to improve performance, strength-training programs that focus on just one or two muscles of the lower leg could be setting individuals up for injury.
The traditional understanding of the lower leg, specifically the gastrocnemius and soleus muscles of the calf, suggests that they work most effectively to create plantar flexion. Toe raises, both with and without resistance, are often recommended as an effective exercise for strengthening these muscles. However, these exercises could be a potential cause of common lower-leg and foot injuries. Yes, the calves can point the toes, but during integrated movements, such as walking or running, they are responsible for controlling motion of the foot as well as supporting mobility of the hip. When it comes to how the muscles of the lower leg function during upright activities such as walking, running and jumping, it is important to know how all of the muscles and joints work together to create successful movement (Table 3). Instead of helping to improve performance, strength-training programs that focus on just one or two muscles of the lower leg could be setting individuals up for injury.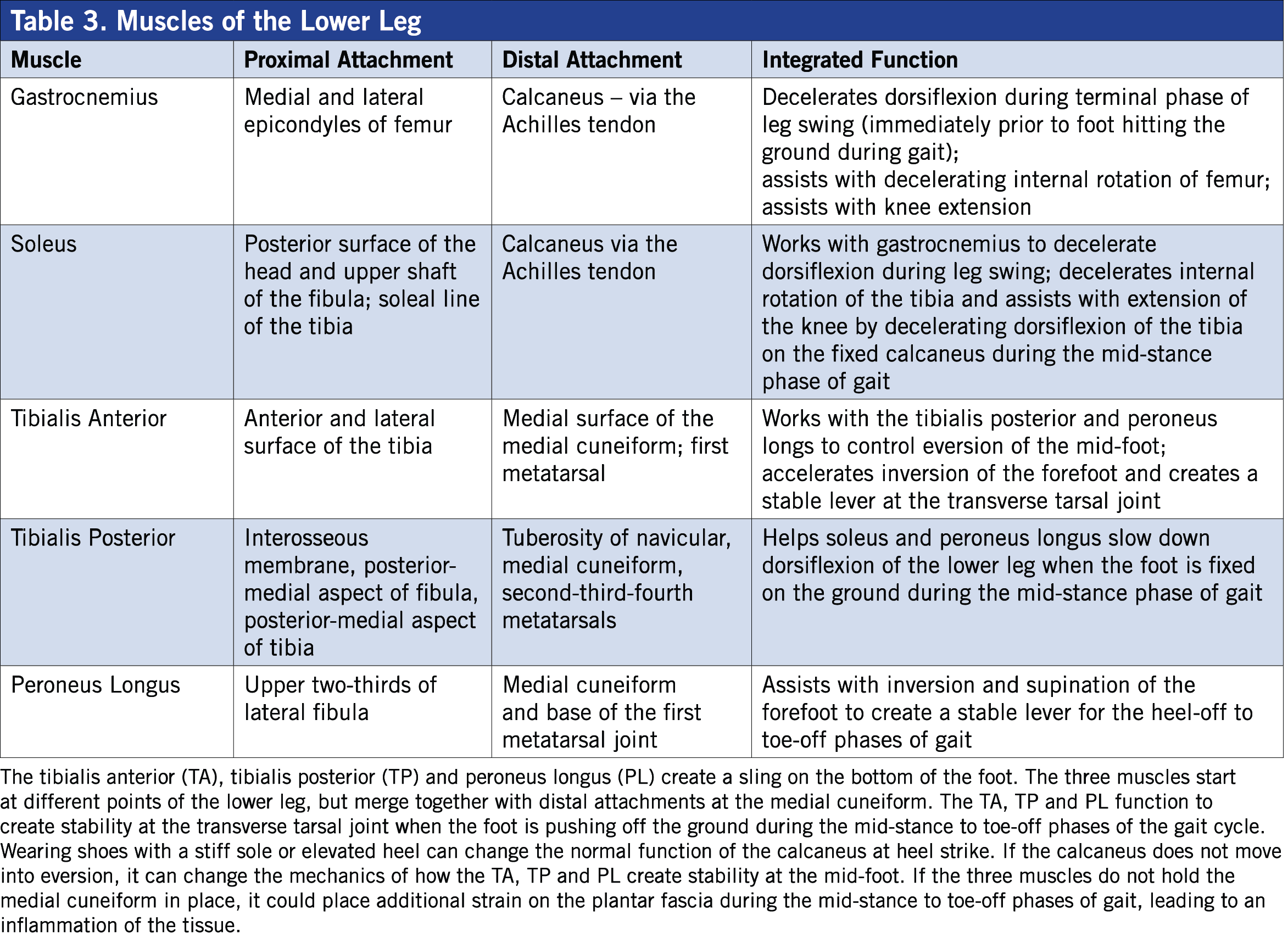
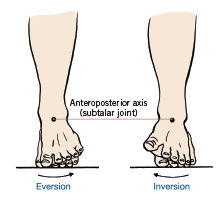 Pronation is a normal motion designed to allow the foot to absorb the weight of the body. During pronation as the foot and lower leg hit the ground, the muscles responsible for dorsiflexing and supinating the foot lengthen eccentrically to decelerate the forces created by gravity and ground reaction. An important shock-absorption mechanism is the medial longitudinal arch, which depresses during the ground-contact and early midstance phases of gait. As the body passes over the foot in midstance, the motion of the foot changes from pronation to supination as the same muscles responsible for decelerating pronation suddenly shorten to lift the medial longitudinal arch to create supination. Pronation allows the foot to be mobile to absorb ground forces. Supination occurs during the later phases of gait, causing the foot to be a solid lever for pushing off against the ground. During the mid-to-later phases of gait, when the foot is changing from pronation to supination, the entire leg changes direction from flexing, adducting and internally rotating to extending, abducting and externally rotating (Neumann, 2010; Gray and Tiberio, 2007). During this normal chain reaction of biomechanics, several muscles in the foot and leg must work together to both absorb and generate force. If the tissues of the foot lose the extensibility and strength to control these forces, it could result in a number of injuries, including plantar fasciitis and Achilles tendon ruptures (Gray and Tiberio, 2007).
Pronation is a normal motion designed to allow the foot to absorb the weight of the body. During pronation as the foot and lower leg hit the ground, the muscles responsible for dorsiflexing and supinating the foot lengthen eccentrically to decelerate the forces created by gravity and ground reaction. An important shock-absorption mechanism is the medial longitudinal arch, which depresses during the ground-contact and early midstance phases of gait. As the body passes over the foot in midstance, the motion of the foot changes from pronation to supination as the same muscles responsible for decelerating pronation suddenly shorten to lift the medial longitudinal arch to create supination. Pronation allows the foot to be mobile to absorb ground forces. Supination occurs during the later phases of gait, causing the foot to be a solid lever for pushing off against the ground. During the mid-to-later phases of gait, when the foot is changing from pronation to supination, the entire leg changes direction from flexing, adducting and internally rotating to extending, abducting and externally rotating (Neumann, 2010; Gray and Tiberio, 2007). During this normal chain reaction of biomechanics, several muscles in the foot and leg must work together to both absorb and generate force. If the tissues of the foot lose the extensibility and strength to control these forces, it could result in a number of injuries, including plantar fasciitis and Achilles tendon ruptures (Gray and Tiberio, 2007).