Darius is a physically active 40-something attorney who enjoys strength-training workouts, basketball and golf. Richard is a 30-something retail manager whose routine includes resistance training, high-intensity interval training and basketball at every opportunity. Besides their shared love of basketball, these two men—along with thousands of other men in their age bracket—have something else in common: significant lower-leg injuries. During a basketball game at his gym, Darius suffered a complete rupture of his Achilles tendon, which took almost a full year to heal. Richard tore the peroneus brevis muscle near its insertion on the bottom of his foot, which required wearing an orthopedic boot to control ankle motion for two months and long-term rehabilitation.
The lower leg and foot are a complex structure of muscles, tendons, ligaments and bones responsible for withstanding significant stresses during upright activities like walking, running and jumping. The lower leg and foot are the interface between the body and the ground. Every time the foot makes contact with the ground, it has to mitigate the forces caused by gravity accelerating the body’s weight downward, and the equal and opposite impulse created by the solid ground. Because of these two competing forces, recreationally active adults, like Darius and Richard, are at risk for injuries of the lower leg and foot, particularly plantar fasciitis and Achilles tendon damage.
Common Injuries of the Lower Leg and Foot
An estimated 75% of American adults will experience foot pain at some point in their lives. In a population of 100,000 adults, at least 18 individuals will experience significant injuries, such as a rupture or tear to the Achilles tendon; most of those injuries (68%) occur during participation in a sport or recreational activity. A majority of individuals who experience a significant injury to the Achilles tendon are athletic men between the ages of 30 and 55. Of all sports-related Achilles injuries, approximately half (47%) were related to basketball; approximately 20% of Achilles injuries are related to daily activities including walking or carrying objects.
The foot and lower leg must have the mobility to manage varying forces and surfaces, yet provide the stability to push against the ground for walking and running. The human ankle and foot contain 28 muscles that control stability and mobility at 33 joints, organized into the rearfoot, midfoot and forefoot (Table 1). According to physical therapist Gary Gray, founder of the Gray Institute, “[Personal trainers] need to understand the role that the lower leg muscles play during gait, specifically how the foot functions when it makes contact with the ground and reacts as the body is passing over it.”
While diagnosing injuries is outside your scope of practice, it’s appropriate—and important—to understand the mechanisms of common injuries so you’re able to design exercise programs that help clients reduce the risk of injury or help them return to their favorite activities after appropriate medical care. Understanding how the foot and lower leg function together during upright movement is essential to building programs that improve strength and resiliency and help clients avoid debilitating injuries that can keep them from their favorite activities.
Biomechanics of the Lower Leg and Foot
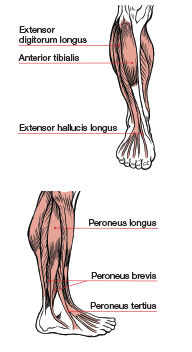
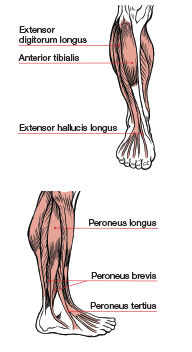
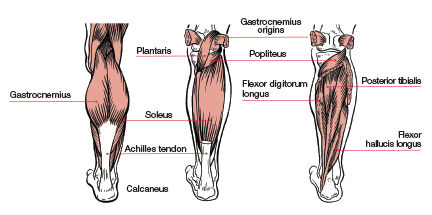
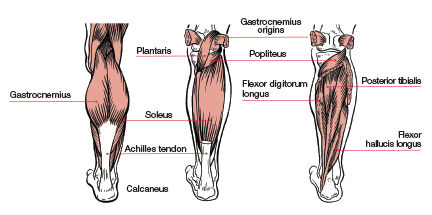
The traditional view of the lower leg, specifically the gastrocnemius and soleus, emphasizes how they work to produce plantar flexion. However, when trained or considered in isolation—e.g., single-joint calf work that ignores foot and hip coordination—they may contribute to common lower-leg and foot injuries. Yes, the calves can point the toes, but during integrated movements, such as walking and running, they also control foot motion and support hip mobility. When it comes to how the muscles of the lower leg function during upright activities such as walking, running and jumping, it is important to know how all of the muscles and joints work together to create successful movement. Programs that focus on only one or two lower-leg muscles may inadvertently set clients up for injury.
This installment of ACE’s muscle mechanics series examines how the lower-leg muscles work as an integrated unit to help the foot convert from a mobile structure during the ground contact phase of gait to a stable lever capable of pushing off of the ground to propel the body forward.
Muscle contains two primary types of tissue: (1) the inelastic contractile elements of actin and myosin responsible for creating a shortening force, and (2) elastic connective tissue and fascia interwoven between muscle fiber. The contractile element initiates the forces required to move bones, while the elastic tissue lengthens in response to applied forces. The lower-leg muscles are an excellent example of how these two properties must work together to create efficient, injury-resistant movement.
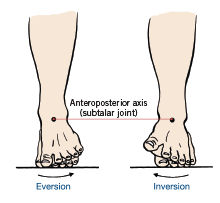
How a muscle functions as it lengthens can, in fact, be more important than its concentric role. The best way to learn how the structures of the lower leg and foot function is to look at what they do during the gait cycle of walking or running. At initial ground contact, the foot undergoes triplanar pronation at the subtalar joint as the talocrural joint adducts and plantar flexes, the calcaneus everts and the tibia internally rotates.
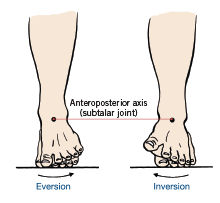
Pronation is normal and allows the foot to absorb impact forces as the body contacts the ground. During pronation, the muscles responsible for dorsiflexing and supinating the foot lengthen eccentrically to decelerate the forces created by gravity and ground reaction. An important shock-absorption mechanism is the medial longitudinal arch, which depresses during ground-contact and the early midstance phases of gait. As the body passes over the foot in midstance, the motion changes from pronation to supination as the same muscles responsible for decelerating pronation suddenly shorten to lift the medial longitudinal arch. Pronation allows the foot to be mobile to absorb ground reaction forces. Supination occurs during the later phases of gait, causing the foot to become a solid lever for pushing off the ground. During the mid- to late phases of gait, when the foot is changing from pronation to supination, the entire leg changes direction from flexing, adducting and internally rotating to extending, abducting and externally rotating. During this normal chain reaction of biomechanics, several muscles in the foot and leg must work together to both absorb and generate force. If the tissues of the foot lose the extensibility and strength to control these forces, it could result in injuries, including plantar fasciitis and Achilles tendon ruptures.
The Achilles Tendon
The Achilles tendon is formed by the gastrocnemius and soleus and attaches to the heel at the calcaneal tuberosity. Injuries are common among middle-aged “weekend warriors” who don’t follow an appropriate program or warm up properly before participating in their favorite activities. Factors that increase the risk of an Achilles tendon injury include age, body weight and activity demands. Explosive movements, such as jumping, landing or making rapid changes in direction, all of which are common during basketball, also raise the risk.
As Darius experienced, a rupture or tear of the Achilles tendon can be extremely painful, and recovery can last up to a year. It’s important to note that most Achilles injuries happen during the spring and summer months, with significantly fewer happening during the winter. What does this mean for health and exercise professionals? If you work with clients who play basketball, tennis or soccer, you can help reduce their risk of injury by implementing an appropriate exercise and conditioning program.
The Achilles tendon is the largest and strongest tendon in the human body, capable of withstanding loads up to 10 times of an individual’s body weight during dynamic activities such as sprinting or jumping. It is hypothesized that a loss of elasticity resulting in muscle-tendon stiffness is a common cause of injury. According to Newton’s third law, for every action there is an equal and opposite reaction. When your foot hits the ground, the downward force of your body weight is transmitted into the ground. At the same time, that ground-reaction force is being transmitted back up into your body. As you quickly transition from ground strike to midstance, the Achilles tendon experiences a rapid lengthening, which is increased significantly during high-speed activities such as jumping or sprinting. The muscles of the lower leg and foot need to be extensible in all three planes of motion to allow proper joint motion to occur during normal upright movements. For very active individuals, however, the tissues of the lower leg and foot need to be specifically conditioned to withstand the high forces produced by rapid changes of direction, jumping and landing. One reason why Achilles tendon injuries may be common among older athletic individuals such as Darius and Richard is that elastic connective tissue of fascia and tendons can lose their elasticity over time.
The Calf as a Core Muscle
Movement of the foot and lower leg has a direct impact on motion of the proximal portion of the femur as it inserts into the iliofemoral (hip) joint of the pelvis. Internal rotation of the tibia creates internal rotation at the iliofemoral joint of the hip. If the calf muscles become overly tight, it can change the motion of both the lower leg and hip joints. This can, in turn, change the length-tension relationships and function of the muscles responsible for controlling motion at the hip.
The gastrocnemius originates on the medial and lateral femoral condyles. Tightness in the calf muscles can change the range of motion of the hip. If the hip loses range of motion, it can change the position of the pelvis and lumbar spine, which will affect the muscles commonly referred to as the core. “During gait, the heel raises off of the ground as a reaction to what the hip flexors do, which is to restrict extension of the femur in the sagittal plane,” explains Gray, “and not as the result of contraction of the plantar flexors.” Understanding how all muscles work together to create coordinated movement is an important component of being a successful fitness professional.
When combined with exercises such as calf raises that focus on the concentric properties of contractile tissue, this natural loss of elasticity can create a clear mechanism for lower-leg injuries. Calf raises can enhance strength and stiffness of the contractile element of lower-leg muscles, but don’t improve the elasticity of the connective tissue of the Achilles tendon or fascia at the plantar surface (bottom) of the foot. An exercise program that focuses solely on the concentric action of plantar flexion during calf raises won’t adequately prepare lower-leg and foot muscles for the rapid lengthening and high eccentric loads of landing and making rapid changes of direction. “We find that exercises that do not reinforce what happens during normal function are not effective at improving the performance of the muscle,” explains Gray, “or the part of the body that muscle is supposed to control.”
|
Table 1. Primary Joints Responsible for Motion of the Foot and Lower Leg*
|
|
Bones
|
Joint(s)
|
Motion(s)
|
|
Tibia
Fibula
Talus
Calcaneus
|
Distal tibia and fibula
Talocrural
Subtalar
|
During dorsiflexion of the talocrural joint, the talus slides posteriorly between the distal tibia and fibula.
When the foot hits the ground, the calcaneus everts in the frontal plane, causing the talus to collapse medially to create motion at the subtalar joint and internal rotation of the tibia and fibula.
|
|
Calcaneus
Navicular
Cuboid
Medial cuneiform
|
Transverse tarsal
Cuneonavicular
|
During the initial phases of gait as the calcaneus and rear foot move into eversion, the transverse tarsal and cuneonavicular joints allow the forefoot to remain fixed on the ground.
|
|
*There are 33 joints in the foot and ankle. This table represents the larger joints involved in normal motion of the feet and legs.
|
|
Table 2. Major Actions of the Ankle and Foot During the Stance Phase of Gait*
|
|
Region
|
Joint
|
Action
|
Desired Function
|
Action
|
Desired Function
|
|
Ankle
|
Talocrural
|
Plantar flexion
|
Allows rapid foot contact with the ground
|
Dorsiflexion followed by rapid plantar flexion
|
Produces a stable joint to accept body weight, followed by thrust needed for propulsion at push-off (toe-off phase of gait)
|
|
Rearfoot
|
Subtalar
|
Pronation and lowering of the medial longitudinal arch
|
Permits internal rotation of the lower leg; allows foot to function as a shock absorber over various surfaces; produces a pliable midfoot
|
Continued pronation changing to supination, followed by raising the medial longitudinal arch
|
Permits external rotation of the lower leg; converts the midfoot to a rigid lever for push-off
|
|
Midfoot
|
Transverse tarsal
|
Relative inversion as a response to ground reaction force
|
Allows full extent of subtalar joint pronation
|
Relative eversion
|
Allows the midfoot and forefoot to maintain firm contact with the ground (as the calcaneus everts)
|
|
Forefoot
|
Meta-tarsophalangeal
|
Insignificant
|
N/A
|
Extension
|
Raises the medial longitudinal arch and stabilizes the midfoot and forefoot for push-off
|
|
The unique structures of the foot allow it to convert from a mobile structure capable of withstanding high ground-reaction forces during ground strike to a stable structure that can generate force by pushing off the ground. The primary joints that allow mobility of the foot as it makes contact with the ground are the subtalar, transverse tarsal and talocrural. Each joint allows movement in a specific plane of motion and all function together to allow triplanar pronation. As the body passes over the foot, the tibia externally rotates and the tibialis posterior, tibialis anterior and peroneus longus contract to pull on the medial cuneiform. This lifts the medial longitudinal arch, creating supination and making the foot a solid lever for propelling the body forward to the next phase of the gait cycle.
Shoes with an elevated heel and stiff sole, including women’s dress shoes and men’s work boots, restrict these normal chain-reaction biomechanics. Shoes that prevent the joints from experiencing their normal motion can change the function of the tissues of the lower leg and foot, which is a potential mechanism for injury.
*Adapted from Neumann, 2010
|
The Soleus Can Extend the Knee
A muscle does not always need to cross a joint to affect motion. For example, the soleus muscle attaches to the tibia and does not cross the knee, yet it can influence motion at the knee. During the midstance to early heel-off phases of gait, the tibia dorsiflexes over a relatively fixed calcaneus. As that happens, the soleus lengthens, which restricts forward motion of the tibia. As the tibia stops moving forward over the fixed calcaneus, the opposite leg swings forward. As this is happening, the knee above the foot in midstance moves into extension. Because the soleus restricts this forward motion of the tibia, it aids in extending the knee during gait.
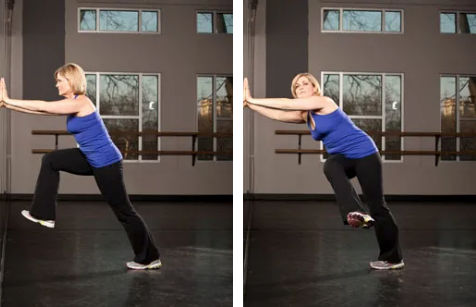
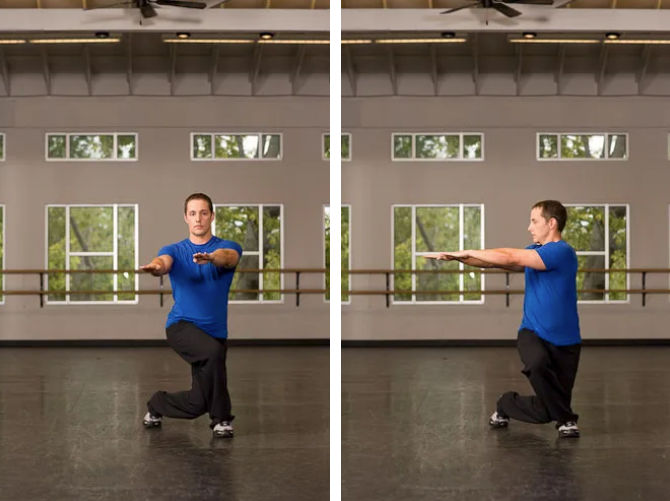
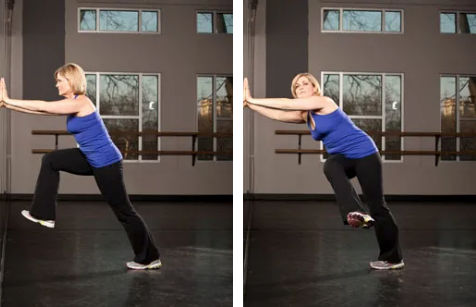
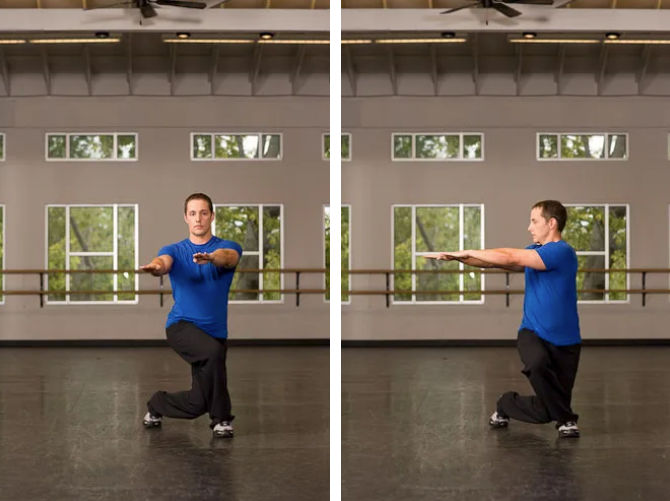
Exercises such as multiplanar lunges with the foot fixed on the ground while the rest of the body moves can improve the extensibility of the soleus, tibialis anterior and tibialis posterior, helping convert from lengthening to shortening, which is how they function during normal gait.
|
Table 3. Muscles of the Lower Leg
|
|
Muscle
|
Proximal Attachment
|
Distal Attachment
|
Integrated Function
|
|
Gastrocnemius
|
Medial and lateral epicondyles of femur
|
Calcaneus via the Achilles tendon
|
Decelerates dorsiflexion during terminal leg swing;
assists with decelerating femoral internal rotation;
assists with knee extension
|
|
Soleus
|
Posterior surface of the head and upper shaft of the fibula; soleal line of the tibia
|
Calcaneus via the Achilles tendon
|
Works with the gastrocnemius to decelerate dorsiflexion during leg swing; decelerates internal rotation of the tibia and assists with extension of the knee by decelerating dorsiflexion of the tibia on the fixed calcaneus during the midstance phase of gait
|
|
Tibialis Anterior
|
Anterior and lateral surface of the tibia
|
Medial surface of the medial cuneiform; first metatarsal
|
Works with the tibialis posterior and peroneus longus to control eversion of the midfoot; accelerates inversion of the forefoot and creates a stable lever at the transverse tarsal joint
|
|
Tibialis Posterior
|
Interosseous membrane, posterior-medial aspect of fibula, posterior-medial aspect of tibia
|
Tuberosity of navicular, medial cuneiform, bases of the 2nd–4th metatarsals
|
Helps the soleus and peroneus longus slow tibial dorsiflexion when the foot is fixed on the ground during the mid-stance phase of gait
|
|
Peroneus Longus
|
Upper two-thirds of lateral fibula
|
Medial cuneiform and base of the first metatarsal
|
Assists with inversion and supination of the forefoot to create a stable lever for the heel-off to toe-off phases of gait
|
|
The tibialis anterior (TA), tibialis posterior (TP) and peroneus longus (PL) form a sling on the bottom of the foot. The three muscles start at different points in the lower leg but share distal attachments at the medial cuneiform. The TA, TP and PL function to create stability at the transverse tarsal joint during the mid-stance to toe-off. Wearing shoes with a stiff sole or elevated heel can change the normal function of the calcaneus at heel strike. If the calcaneus does not move into eversion, it can change the mechanics of how the TA, TP and PL create stability at the midfoot. If the three muscles do not hold the medial cuneiform in place, it could place additional strain on the plantar fascia during the mid-stance to toe-off phases of gait, leading to inflammation.
|
Strength Training for the Lower Leg and Foot
Proper strength training should support the normal biomechanics that allow the foot to convert from mobility to stability and increase the elasticity of the fascia and connective tissue. It is also important to use exercises that involve the whole leg to improve how all the joints, from the transverse tarsal in the midfoot to the iliofemoral joint of the hip, function together during upright movements. For example, proper hip extension relies on the tibia dorsiflexing over the foot when it is fixed on the ground during the midstance phase of gait. The only way to improve this is to train with movements that involve all of leg joints together. Standing on one leg and moving the body in all planes of motion using toe touches, lunges and bounds (leaping from one foot to the other) can be extremely effective for strength training and injury prevention.
When introducing dynamic lower-leg exercises, start with a limited number of repetitions and sets to allow fascia and elastic connective tissue to adapt to the rapid lengthening before progressing volume. In normal, asymptomatic tissue, progress over about six to 10 weeks from single sets of four to eight repetitions to multiple sets of 10 to 15 repetitions (on each leg).
|
Table 4. Workout Program for Muscles of the Lower Leg and Foot
|
|
|
Exercise
|
Description
|
Reps*
|
Sets*
|
Rest Interval
|
|
Standing Ankle Mobilization
|
Place both hands on a wall. Keep the right leg extended with the heel on the floor as you lift the left leg and swing it right and left to lengthen the Achilles while the heel stays flat on the floor.
|
6–15 swings each leg
|
1–3
|
N/A
|
|
Single-leg Balance With Lateral Toe Touch and Cross-body Reach

|
Balance on the left leg; reach the right leg directly out to the side (3 o’clock position) while the left hand reaches to 9 o’clock position). Repeat on both sides.
|
6–15 each leg
|
1–3
|
30 seconds after both legs
|
|
Opposite Side Lateral Toe Touch With Overhead Lateral Reach

|
Stand on the left leg and reach across the body with the right leg to 9 o’clock while reaching overhead with the left arm to train supination with the foot on the floor.
|
6–15 each leg
|
1–3
|
30 seconds after both legs
|
|
Side Lunges to Glute Activation Lunges

|
Combine a right-side lunge immediately followed by a glute-activation lunge (right leg moves behind left) to train the foot’s transition from pronation (side lunge) to supination (glute activation).
|
6–15 each leg
|
1–3
|
60 seconds after both legs
|
|
Transverse Plane Lunge

|
Stand with the feet hip-width apart, dumbbells at sides. Keep the left foot at 12 o’clock; step the right foot back/out to approximately 4 o’clock. As the right foot lands, push back into the right hip and reach toward the right foot, then return to center. This exercise improves mobility/strength of the lower-leg supinators during midstance and integrates foot-ankle-knee-hip mechanics in the transverse plane.
|
6–15 each leg
|
1–3
|
60 seconds after both legs
|
|
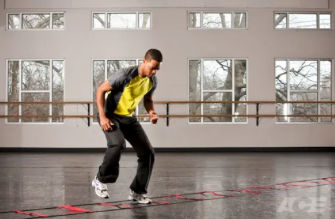
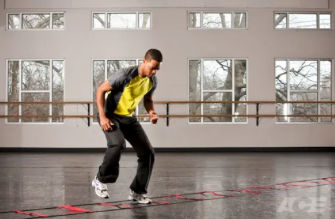
Lateral Agility Ladder
|
Start in an athletic stance. Move laterally down the ladder, emphasizing landing through the full foot (ball to heel) to lengthen the Achilles; perform an equal number of reps in both directions.
|
1 ladder pass
|
1–5
|
30 seconds after both directions
|
|
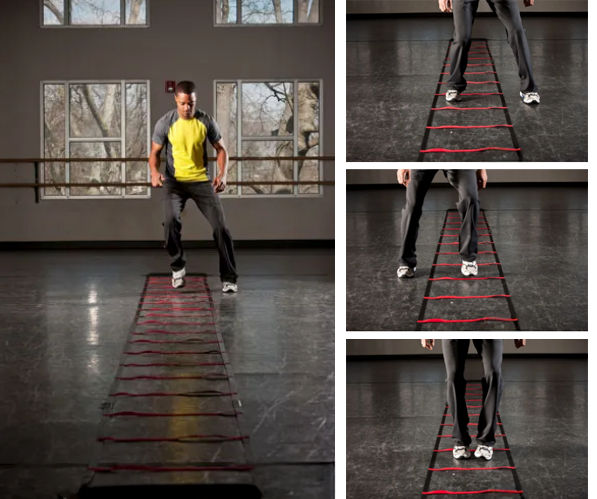
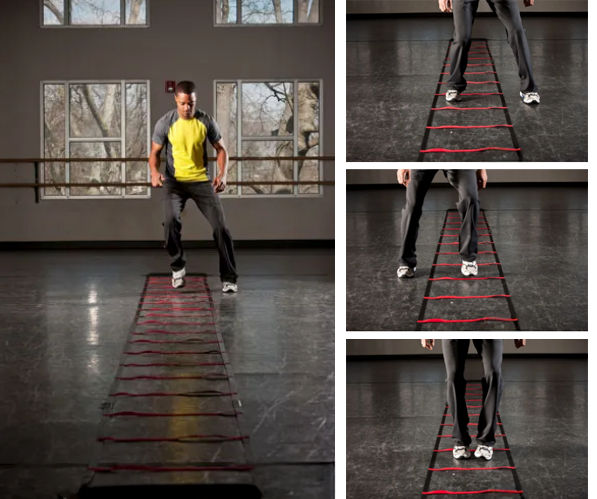
Multidirectional Ladder Drill
|
Stand left of the ladder in an athletic stance. Move the arms in opposition to the legs. The foot pattern is: (R)in-(L)in-(R)out-(L)in-(R)in-(L)out. Allow the foot to roll fully to the floor to maximize Achilles lengthening each time the foot hits the floor.
|
1 ladder pass
|
1–5
|
30 seconds after down and back
|
|
When starting this program, use fewer repetitions and one set per exercise. Gradually progress to three sets over the course of six to 10 weeks.
|
Conclusion
When told about the need to train the elastic component of soft tissue, Darius immediately recognized his mechanism of injury. He had been wearing stiff-soled dress shoes and, on arriving at the gym, jumped straight into a basketball game without a proper warm-up. Since returning to his routine, Darius has made mobility training a key component of his workouts and credits it with keeping him active. Before he hops on the court or plays a round of golf, Darius performs movement patterns in all three planes of motion to ensure he is ready to begin. Understanding how the lower leg and foot function can help you keep your clients and group fitness participants injury-free and engaged in their favorite activities.





 by
by