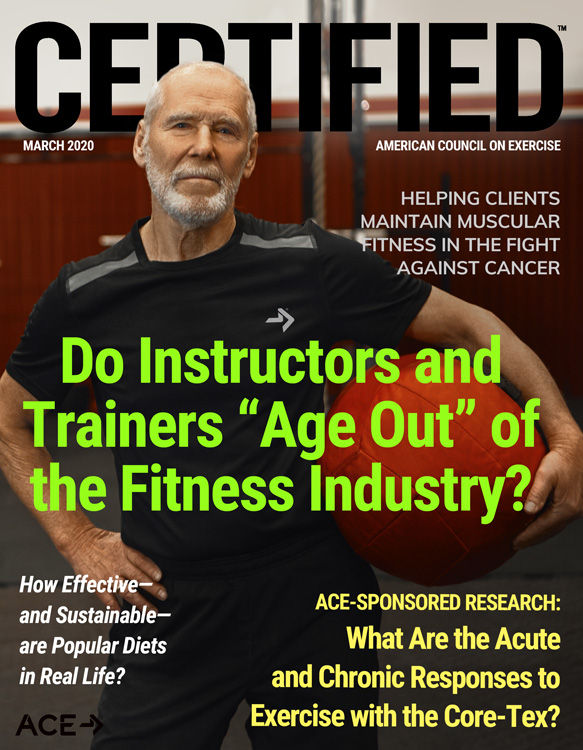
Ready for some good news? A bright spot of the new decade was the announcement of the greatest single-year improvement in overall cancer survival rates. This reduction in mortality of 2.2% was the largest single-year decline since a peak in 1991. Additionally, the overall survival rate has improved by 29%, resulting in 2.9 million fewer deaths in the past 30 years (Siegel, Miller and Jemal, 2020).
If you are a health and exercise professional who has worked with cancer survivors, you may view these statistics through a slightly different lens. While it’s exciting to learn that there are nearly 17 million cancer survivors in the United States today, your clients are likely experiencing the physical and emotional fallout of cancer treatment. In addition to the numerous side effects these individuals endure, many also lack confidence in their own bodies with regard to both ability and safety. The exercise programs that they once were able to do may not feel the same or elicit the same results or are simply no longer appealing. This leads to not only frustration but lack of compliance, which is one of the most important elements of fitness success.
It might seem contrary to common sense that someone with cancer would continue or even start an exercise program. However, it is important to note that the most recent guidelines from the American College of Sports Medicine (ACSM) and the American Cancer Society (ACS) recommend that anyone affected by cancer should avoid physical inactivity and participate in a regular exercise program. (Learn more about these recommendations in this earlier CERTIFIED article: KISS Cancer With Exercise: Simple Principles to Guide Health and Exercise Professionals.)
In addition to the exercise recommendations, all survivors are advised to obtain and maintain a healthy weight, given that obesity is linked to increased rates of recurrence and other comorbidities such as cardiovascular disease and joint-related orthopedic concerns [National Comprehensive Cancer Network (NCCN), 2019; Arnold et al., 2016]. Sedentary behaviors, lack of exercise, weight gain, and other adverse physical and functional side effects are all related to loss of lean muscle mass. Helping cancer survivors maintain lean muscle mass in the fight against cancer is a prime role for health and exercise professionals.
The Impact of Cancer on Lean Muscle Mass
For someone affected by cancer, scale weight takes on a different meaning than simply aesthetics. Individuals with cancer are often told not to lose weight during treatment as it could be interpreted as disease progression. However, it is not uncommon for individuals to be secretly happy that they are losing weight because they report that they often “need to” lose weight. This back-and-forth tug of opposing goals puts patients in a confusing place as they want to live well but are often frustrated with their physical function and appearance after cancer treatment. Given that the average age of a cancer diagnosis is 66 years old, many of these individuals have already experienced sarcopenic changes and weight changes through their lifespan [National Cancer Institute (NCI), 2015].
Many people are programmed from an early age to view the number on the scale as a measure of physical health, and it often impacts self-perception and mental health. Add a cancer diagnosis into the equation and the preoccupation with weight becomes more magnified and misperceptions even more compounded. Is weight really the right measure? What other variables might be important to consider and attend to?
Sarcopenia, Osteopenia and Cancer
Advances in technologies that assess various aspects of health and fitness have created greater opportunities for obtaining and tracking key health metrics and have decreased reliance on scale weight and body mass index (BMI) as primary measures for program success. Unfortunately, the healthcare industry has a pattern of over-relying on the metric of BMI only, which is often misinterpreted, driving individuals to rely solely on weight-loss programs as a means to improve health. However, the number on the scale is just one piece of the puzzle. Body composition is made up of a variety of components, including fat, water, bone, organs and lean muscle.
Through the aging process, decreased intake of quality nutrition and an increase in sedentary behaviors, body composition begins to move in a less favorable direction. Sarcopenia, the normal loss of muscle that happens with aging, begins to accelerate and the effects become more cumulative. Bone mineral density also decreases as the bones lose mass from decreased calcium and other minerals. Hormone changes linked to menopause, birth control and cholesterol-lowering statins all contribute to loss of bone. The body begins to store more fat in unhealthy areas such as the abdomen, and there is fat infiltration in the bone and muscle. In addition to changes from aging, loss of muscle strength and function from lack of activity is often one of the most significant factors contributing to body-composition changes. These physical changes also lead to many functional concerns, such as loss of balance or the ability to make simple daily movements such as getting in and out of a chair or up and down stairs without assistance.
A diagnosis of cancer accelerates the typical sarcopenic process. Changes in lifestyle, cancer treatments and side-effect management (medication) all accelerate the process. Additionally, there are often potential long-term physical changes such as hormone status (e.g., chemotherapy may cause early menopause) or removal and treatment of organs affecting virtually every aspect of an individual’s life. Add in the emotional toll a cancer diagnosis has and the impact is life-altering and the person diagnosed enters into a “new normal.”
Within the first year of a cancer diagnosis, the vast majority of patients experience a noticeable reduction of activity in comparison to their healthy counterparts (Schmidt et al., 2017). This happens due to a variety of factors, including doctors and treatment appointments, fatigue or other side effects from treatment, and a lack of confidence that they should be continuing to exercise or remain in a group exercise program. Many patients also have one or more surgeries, which may require periods of inactivity to allow the body to heal. Sedentary behavior is the single biggest contributor to loss of lean muscle mass.
Not only do patients expect their oncology team to tell them to exercise (Hardcastle et al., 2018), many of the patient-support organizations reiterate talking to their doctor before beginning any exercise program. Most physicians are not trained to provide this guidance and tend to err on the side of caution, often encouraging walking for exercise. Unfortunately, walking may actually be unsafe for some individuals, such as those with neuropathy, which results in a loss of sensation in the hands or feet. Additionally, walking does not improve fatigue due to the lack of recruitment of Type II muscle fibers, which is the primary fiber type that is lost if not regularly recruited.
The most recent cancer exercise guidelines highlight the importance of resistance training. Following general muscle fitness guidelines, which includes lifting weights for at least one set of eight to 12 repetitions with a one-minute rest between sets, is both beneficial and important in working with clients who have had a diagnosis of cancer. It is important to recognize physical changes, such as:
- Weak core muscles after a colon resection surgery or ovarian cancer removal
- Scar tissue in the chest from breast surgery and reconstruction
- Weak pelvic floor and lower-back muscles from rectal cancer surgery and radiation requiring more sedentary and restricted behavior
While these are pieces of the larger puzzle of a client’s fitness and function, it does not mean he or she should avoid exercise or movement. Understanding an individual’s limitations is a key part of the intake process and helps identify appropriate modifications. As a health and exercise professional, your job is to do the research necessary to help the survivor achieve his or her goals and to communicate confidence in coaching or instructing a resistance-focused regimen.
Cancer survivors also benefit from workouts that increase their heart rate to reduce cardiovascular side effects or other comorbidities. Workouts that incorporate high-intensity interval training (HIIT), functional strength work or other intervals that include resistance while bringing the heart rate up should be the base of the client’s program. Exercise programming should be adapted to the client’s individual needs and potential limitations, but even a chair-based HIIT program can be delivered with some creativity.
When working with a client or class participant, it is important to guide him or her through exercises that may be more physically or emotionally challenging, with correct form as a priority. Always focus first on range of motion before adding load and be sure to review the right and wrong types of pain to expect from exercise. Cancer pain is one of the most common concerns and fears, particularly when there has been a recurrence or disease progression. Exercise is a great way to help survivors stay in tune with their bodies and consistently engage in how their bodies move and feel.
Exercise should always be adjusted according to how a client feels on any given day, recognizing when to push forward and when to back off. Additionally, each time you see the client is an opportunity to ask specific questions:
- What are your fitness-related goals for today, this week or this month?
- How did you feel after our last workout?
- How is your energy today?
- Any physical changes since we last worked together?
- Are you experiencing any different or worse side effects than our other exercise sessions?
These questions are especially helpful when you are working with someone who is undergoing treatment such as chemotherapy or living with advanced cancer.
A Sample Workout Program for Different Fitness Levels
What follows is an example of a resistance-based + HIIT functional-exercise program for three different fitness levels: foundational, standard and highly functional.
- Foundational: Clients at this level have not been doing any planned exercise. They have some functional limitations, such as balance or difficulty moving from a seated to standing position. In addition to general weakness, they may have physical limitations or be severely deconditioned. Walking into an exercise facility is generally taxing.
- Standard: These clients do not struggle with activities of daily living and may do some light or inconsistent exercise. They have few if any physical limitations, may be deconditioned or have no history of resistance training. Their biggest complaint is fatigue.
- Highly Functional: These clients have general fitness levels or abilities and are experiencing limited side effects. They are often more interested in metabolic programs and body-composition changes may be their primary goal.
|
Foundations
|
Standard
|
Highly Functional
|
|
Move in a circuit fashion. Rest between sets so heart rate returns to normal.
|
Complete 2−3 sets as a circuit with minimal rest.
|
Combine resistance exercise with high-intensity interval training (HIIT) exercise for a circuit. Used timed circuits to increase heart rate.
|
|
Chair or bench sit to stand (add assistance as needed)
|
Body-weight squat, adding weight once full range of motion has been obtained
|
Weight-loaded squat
|
|
Seated shoulder press; use a broomstick until full range of motion is obtained, then add weights (Note: Encourage clients to keep eyes forward and maintain a neutral spine to engage posterior muscles appropriately.)
|
Standing shoulder press followed immediately by plank with knee tap (can be elevated to box/bench)
|
Thruster using free weights, kettlebell or barbell
|
|
Banded forward march; place a long resistance band around client’s waist and have client march against resistance. Instruct client to increase knee drive and arm swing while moving farther away from you.
|
Box step-up (and over)
(Note: Progress to adding weights and traveling over and down a box as the client becomes stronger. If the client has neuropathy in the feet, place the box near a sturdy place for balance.)
|
Squat jump or box jump
|
|
Elevated push-up on countertop or elevated barbell on rack (Note: Choose an appropriate level of elevation based on the client’s current abilities.)
|
Burpee or up-down with jump to ceiling at top position
|
BOSU squat jump with push-up
|
|
Glute bridge
|
Single-leg Romanian deadlift
|
Inchworm (Note: Push-up is optional.)
|
|
Lying pullover; start with an unweighted object and focus on range of motion. The client must be able to lie flat (Note: Alternate with standing straight-arm pull-down if needed.)
|
Plank (elevate on box or bench as appropriate)
|
Floor plank with alternating foot tap
|
|
Reverse medicine ball slam
|
Kettlebell swing − arms to parallel
|
Kettlebell swing − full range of motion
|
|
Row with a towel attached to a pole
|
Ring/TRX row or inverted pull-up on a Smith machine
|
Jumping pull-up from a box or bench
|
|
Odd object carry
|
Farmer’s carry
|
Kettlebell deadlift x 10 + farmer’s carry
|
Conclusion
The rate of individuals surviving cancer is on the rise, but they are often living with a multitude of side effects that have the potential to impact their ability to live their best lives. Fortunately, the research is clear that there are options for survivors to ameliorate the side effects and build strength, stamina and muscle. The door is wide open for health and exercise professionals to join the medical community in the fight against cancer and have a positive impact on the lives of millions of people.
References
Arnold, M. et al. (2016). Obesity and cancer: An update of the global impact. Cancer Epidemiology, 41, 8–15.
Hardcastle, S.J. et al. (2018). Knowledge, attitudes, and practice of oncologists and oncology health care providers in promoting physical activity to cancer survivors: An international survey. Supportive Care in Cancer, 26, 11, 3711–3719.
JafariNasabian, P. et al. (2017). Aging human body: Changes in bone, muscle and body fat with consequent changes in nutrient intake. Journal of Endocrinology, 234, 1. R35−R51.
Kalyani, R. R., Corriere, M. and Ferrucci, L. (2014). Age-related and disease-related muscle loss: the effect of diabetes, obesity and other diseases. The Lancet Diabetes & Endocrinology, 2, 10, 819–829.
National Cancer Institute (2015). Age and Cancer Risk.
National Comprehensive Cancer Network (2019). NCCN Guidelines Insights: Survivorship Featured Updates.
Schmidt, M.E. et al. (2017). Self-reported physical activity behavior of breast cancer survivors during and after adjuvant therapy: 12 months follow-up of two randomized exercise intervention trials. Acta Oncologica, 56, 4, 618–627.
Siegel, R.L., Miller, K.D. and Jemal, A. (2020). Cancer statistics, 2020. CA: A Cancer Journal for Clinicians, 70, 1, 7–30.





 by
by