As someone who has chronic pain due to arthritis, I’m always looking for drug-free ways to manage it. Chances are, you’ve got clients who also struggle with chronic pain—or maybe you experience it, too.
But what exactly is chronic pain? What causes it? And what interventions currently exist to help it? This article answers these questions and offers guidance on how to help clients manage chronic pain.
An Overview of Chronic Pain
Pain is the body’s way of signaling that something is wrong and that we need to do something about it. When we incur an injury, acute inflammation goes to work to start the healing process.
But what about the pain that doesn’t go away?
According to the Centers for Disease Control and Prevention (CDC), chronic pain is pain that lasts for three months or longer. In 2021, the CDC estimated that 20.9% of adults in the United States—or 51.6 million people—had chronic pain. And 6.9% of the U.S. population experienced high-impact chronic pain, which is pain that has substantially limited one’s life or work activities.
The CDC also states that chronic pain has been linked to other conditions, including depression, dementia (including Alzheimer’s), increased suicide risk, and substance use and misuse.
And chronic pain is costly. According to a 2019 JAMA Network Open article, chronic pain costs an estimated $560 billion to $635 billion each year. These numbers include direct healthcare costs, days of missed work, hours of missed work and lower wages.
For centuries, it was assumed that all pain had a biological root. This idea was the primary basis of many pain theories, starting with Plato and continuing through the late 1970s, when the theory of a biopsychosocial model emerged.
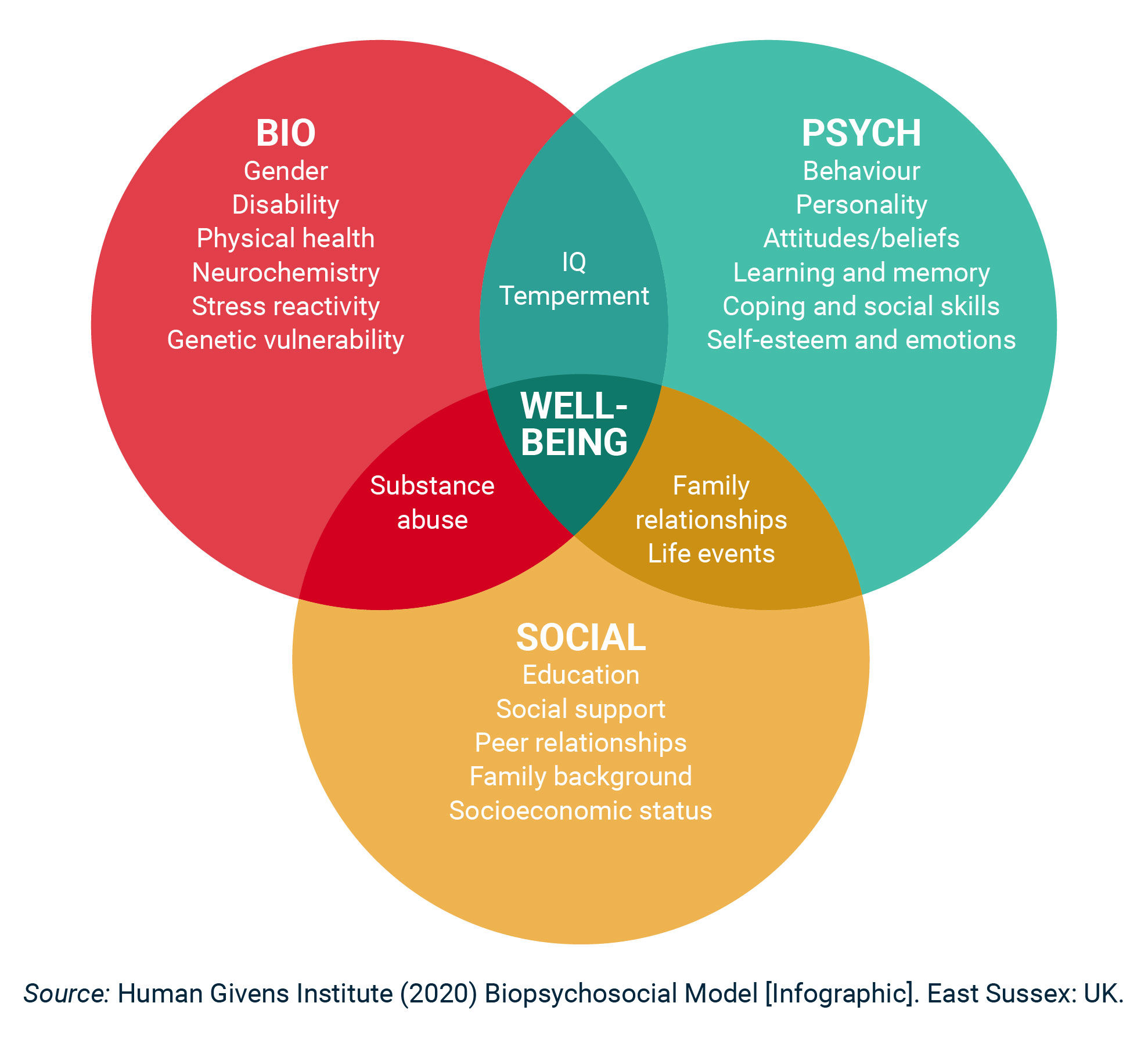
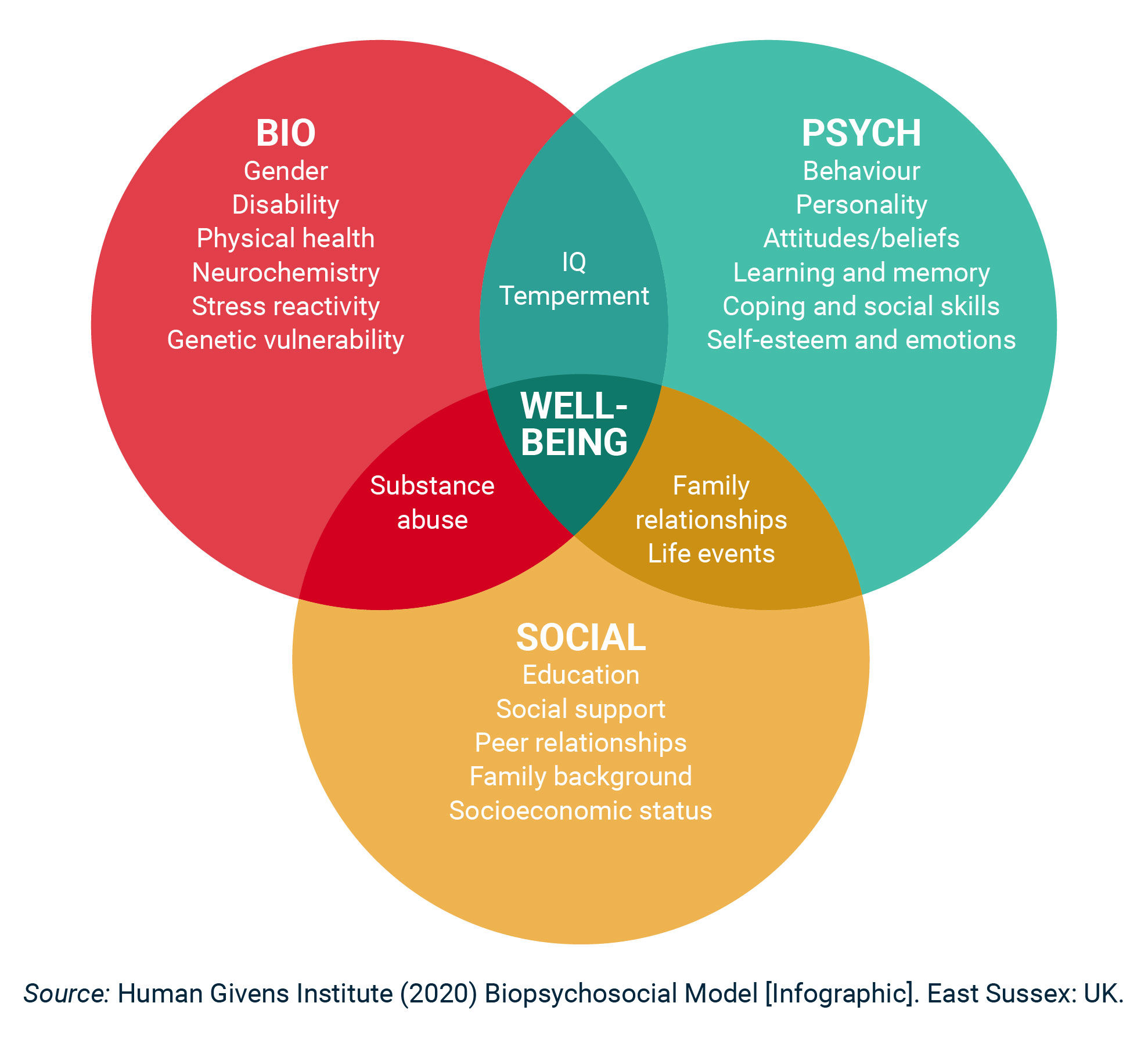
Per a 2021 review in Psychological Science in the Public Interest, the biopsychosocial model suggests that there is an intricate interplay between biological, psychological and social factors that affect one’s health and illness, including pain and its management (Figure 1). This is the foundation of health psychology.
Figure 1. The Biopsychosocial Model of Health
“Chronic pain can be instigated by a myriad of factors, including traumatic injury, stress and anxiety, or a chronic health condition, like arthritis,” explains Lynne Olsen, Corrective Exercise Specialist and Yoga Medicine Therapeutic Specialist. “It can also be more insidious factors like an altered length-tension ratio of muscles, adhesions between layers of tissue, compressed nerves, compensatory patterns and overuse.”
Specifically, says Wayne Lamarre, MEd, LAT, ATC, clinical professor and director of the athletic training program at the University of New England, “some of the most common causes [of chronic pain] include musculoskeletal pathology, systemic dysfunction—like irritable bowel syndrome—and conditions such as fibromyalgia and rheumatoid arthritis.”
So, if pain potentially involves several facets—including physical, psychological and social—that means that pain management should, too.
Unfortunately, many people are only offered pain medications, including opioids, which carry considerable risks, even though published guidelines for treating chronic pain include many non-pharmacological methods.
Before we consider various pain interventions, let’s take a closer look at what pain really is.
Pain 101
You may remember being taught in biology class that the human body has pain receptors. Like many other aspects related to human biology, this belief has been challenged through the years.
“Contrary to common belief, we don’t have pain receptors in our body,” explains Olsen. “Instead, we have nociceptors, which are sensors that detect extreme changes in temperature, pressure and chemicals. Nociceptors send messages to your brain and, ultimately, it’s your brain that filters and interprets them.”
Olsen goes on to say that if your brain interprets a stimulus as a threat, then you will experience pain. “The interpretation, or filter, is based upon your past experiences, your fears, your education about pain, and your beliefs,” says Olsen. “For example, if you’re stressed out and believe that your lower back is vulnerable and fragile, your nervous system will look for information to support that belief and you’re more likely to experience pain. Pain is an output from your brain, not an input to your brain.”
Jacob Teitelbaum, MD, author of several books, including Pain-Free 1-2-3 (McGraw Hill, 2006) and From Fatigued to Fantastic (Avery, 2021), concurs. “Pain is not an outside invader, like an infection,” explains Teitelbaum. “Rather, it is like the warning lights on our body’s dashboard, telling us that something needs attention.”
As a health and exercise professional, this is where you can play a role. But before we jump into each area, remember that, unless you have the credentials, it is outside your scope of practice to diagnose the cause of clients’ pain. Treatments also need to be within your scope of practice. There is no shame in going to the appropriate professionals and asking for advice or referring out to them. Rather, this is your professional responsibility.
Sources of Pain and How to Address Them
When considering where to start with clients who have chronic pain, Olsen says that it’s important to consider the cause of their pain (see sidebar for an assessment). “In my experience, that’s not always as straightforward as you might hope!”
Olsen offers an example of a client who had chronic low-back pain that persisted for over three years, starting in 2020. “Incidentally, the onset of her pain coincided with being blindsided by a divorce, facing the new threat of COVID and having two young kids to raise. Upon our initial assessment, she told me that her back pain was caused by raking leaves one day for several hours.”
This example brings up several questions, says Olsen. “Was her pain caused by her stress and anxiety or by a tight muscle? Maybe both, but it’s important to consider the less-than-obvious influences. Pain doesn’t always equate to physical damage.”
“There has been a significant amount of research published in the last three to five years that suggests a strong correlation between a patient’s psychological construct of a painful event and the level of nociception or pain perception,” explains Lamarre. “The areas of our brain that help to interpret and process the information being received from our nerve endings via the spinal cord can also be influenced by other things, like short- and long-term memory, anxiety and depression levels, etc.”
Physical pain can be helped by numerous modalities, including “nerve flossing, myofascial release, strengthening inactive muscles and lengthening overactive muscles,” says Olsen. (Note: Nerve flossing, also known as nerve gliding or nerve mobilization, is a therapeutic technique used in physical therapy and rehabilitation to address issues related to nerve mobility and flexibility. The goal of nerve flossing is to alleviate symptoms caused by nerve compression or irritation.)
Lamarre agrees and says that health and exercise professionals can have a positive influence on their clients’ discomfort levels after clients have sought an evaluation from their healthcare provider to determine the cause of the pain. Lamarre’s top suggestions include low-impact exercises, like aquatic rehabilitation; massage; myofascial techniques, like foam rolling; and the application of therapeutic heat or cold. “The use of cold treatment, in particular, can still be beneficial in reducing chronic pain levels far after the initial injury,” adds Lamarre.
Lifestyle factors can affect pain, as well. Research, including a 2023 review in Frontiers in Psychiatry, suggests a bi-directional relationship between chronic pain and sleep. People with chronic pain tend to not sleep well, and a lack of quality sleep increases pain. And, a 2023 review in Frontiers in Pain Research suggests a strong link between chronic stress and chronic pain.
Considering Olsen’s client, it’s difficult to know if her chronic pain was solely caused by raking or if the stress of the divorce contributed to it—or perhaps a previous trauma that was triggered by the divorce. In either case, her nervous system was put on high alert.
John E. Sarno, MD, spent his medical career studying how the mind affects the body. In his book, The Divided Mind (Harper Perennial, 2007), Sarno writes, “Almost all of the common pain disorders that have afflicted millions through the years are psychosomatic.”
Psychosomatic refers to what we more commonly hear as being the mind-body connection. And whether you believe Sarno’s conclusion or not, “there is a brain-body connection that cannot be denied,” says Olsen. “Even if you don’t suffer from anxiety, you’ve felt this brain-body connection.”
Olsen goes on to give the example of public speaking, which, for many people, causes their heart to race, breath to become shallow and palms to start sweating. “Your thoughts about that presentation cause a physiological reaction in your body. Something similar happens with pain. Our thoughts, beliefs and fears about pain can greatly influence our experience of it.”
Hence, the nervous system is put on high alert when it perceives a threat. “Simply speaking, a more stimulated or heightened nervous system correlates with pro-inflammatory responses, whereas a more regulated nervous system instigates a more anti-inflammatory response,” Olsen explains. “If we can positively affect the nervous system, we can positively affect one’s experience of pain. Guided meditation, breathing exercises and restorative yoga can all be potent tools for working with pain.”
Numerous studies suggest psychological interventions that can help people with chronic pain. For example, a 2020 review in Psychology and Health and a 2022 review in Pain Medicine suggest that positive psychology interventions can improve the mental health of people with chronic pain by reducing depression, anxiety and stress symptoms, and increasing feelings of well-being.
Researchers explain that negative emotions can contribute to an exacerbation of pain. Helping clients focus on more positive emotions can serve to take the focus off their pain—and their limitations as a result of the pain. It also helps calm and regulate the nervous system, which has been shown to reduce pain perception.
Olsen also urges health and exercise professionals to be mindful about the language they use. “Cues like, 'Be careful not to arch your back or you might bust a disc,' can instill fear. Instead, try cues that remind clients of their body's inherent resilience.”
With guidance from a client’s medical team, slowly introducing “safe” movements can be a way to help clients begin to feel more confident and less fearful of experiencing pain with certain movements. “For example, if you have a client who experiences pain with 170 degrees of shoulder flexion, try taking them to 90 degrees of flexion and stopping there for a few weeks,” urges Olsen. “This gives them an opportunity to experience pain-free movements that build their sense of safety and confidence, both in themselves and you."
The aforementioned review in Psychological Science in the Public Interest found evidence for several other psychological strategies for chronic pain that improve mental health, as well as physical function. A few of the interventions that may be appropriate for health and exercise professionals include relaxation training, cognitive-behavioral therapy techniques and mindfulness-based interventions.
The third factor of the biopsychosocial model is the social aspects of one’s life. There is a lot of evidence, including a 2021 study in General Hospital Psychiatry and a 2022 study in the Journal of the American Geriatrics Society, showing a correlation between chronic pain and social isolation or loneliness. The question is, which comes first—loneliness or pain? Perhaps it doesn’t matter, as the remedy to either is to integrate greater socialization.
It's easy to brush off clients’ complaints of pain and take a “suck it up” or “no pain, no gain” attitude. But this isn’t the most productive path to take.
“Begin with empathy and understanding,” recommends Teitelbaum. “Unfortunately, our modern healthcare system often treats people in chronic pain as if they are malingerers or drug seekers. This adds an enormous emotional toll to their physical suffering. Let them know you understand how difficult their pain is and are here to help.”
As health and exercise professionals, “there’s a lot we can do to support our clients in resolving their pain,” concludes Olsen. “It all starts with listening and asking good questions.”
Pain Assessment
The Pain Academy is a great resource to share with your clients. Here, they can do a fully guided pain self-assessment and receive a movement program tailored to their needs that you can help adjust according to their unique needs and goals.
Expand Your Knowledge
ACE Corrective Exercise Specialist Program
Injuries and chronic conditions can have a devastating impact on an individual's lifestyle. As an ACE Corrective Exercise Specialist, you will help clients regain function and return to normal movement. You will coach clients to improved function, mobility, stability and strength, which will lead to less pain, better health and increased all-around quality of life. You will be equipped to work with a wide variety of clients, from those who want to jump back into an exercise regimen quickly to those who are afraid of moving and reinjuring themselves.
Corrective Exercise Training Essentials – Course Bundle
While some clients have aesthetic and performance goals, many may want help alleviating aches and pains so they can feel empowered in other areas of their lives. Whether it’s joint pain, chronic pain or injury, the Corrective Exercise Training Essentials course bundle will give you the strategies you need to help clients safely and effectively move and feel better with corrective exercise.





 by
by