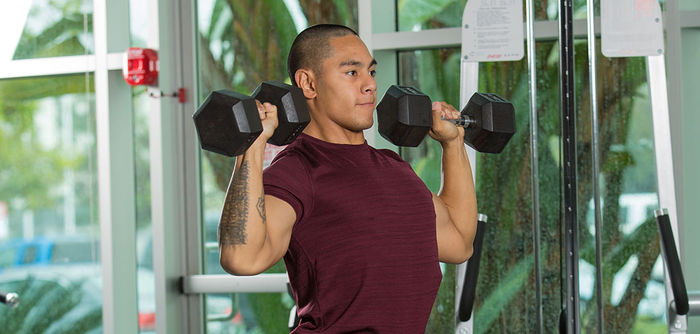
The Importance of Proper Recovery

Proper recovery can be the difference between long-term exercise adherence and burnout or injury. Read what two ACE experts have to say about recovery and try a 10-move active recovery routine that is perfect for those days when you need a break from high-intensity exercise.
Read More