Yoga has become a popular activity in the United States, with approximately 13.2% of the adult population reporting that they have practiced yoga at some point during their lives (Cramer et al., 2016). The most commonly reported reasons for participating in yoga include maintenance of health and wellness, disease prevention, improvement in energy levels, increased immune function and management of conditions such as back pain, stress and arthritis (Cramer et al., 2016). In addition to the general population, there is a growing body of evidence to support participation in yoga for breast cancer survivors.
Breast cancer survivors can experience negative side effects from cancer treatments, including losses in strength, physical function and fatigue (Sehl et al., 2013; Simonavice et al., 2011; Stasi et al., 2003). In addition, swelling, weakness and pain in the affected arm (the arm on the side where the cancer was present) may persist following surgery, radiation and the removal of lymph nodes under the arm (Warmuth et al., 1998). These changes can negatively impact overall quality of life.
However, research has shown that practicing yoga can be beneficial in reducing some of these treatment-related side effects. Studies have reported improvements in physical well-being (Moadel et al., 2007), fatigue (Bower et al., 2012; Moadel et al., 2007), affected arm symptoms (Andysz et al., 2014) and quality of life (Andysz et al., 2014; Culos-Reed et al., 2006) following short-term yoga interventions. In addition, a systematic review and meta-analysis that included 13 yoga interventions in cancer patients concluded that yoga resulted in positive effects on distress and anxiety as well as moderate improvements in fatigue, health-related quality of life, emotional function and social function (Buffart et al., 2012).
Special Considerations for Postures and Class Sequencing
A specific yoga program that is optimal for breast cancer patients and survivors has not been determined, as the yoga interventions implemented in the aforementioned studies varied in frequency, intensity, sequencing and selected postures. Therefore, when determining the appropriate frequency and intensity, and selecting postures for your breast cancer participants, there are several considerations to keep in mind:
- Arm Symptoms: Participants may experience pain, weakness and decreased range of motion in the affected arm as a result of cancer treatments, and the development of lymphedema, which can occur from an accumulation of lymph fluid in the arm (Sakorafas et al., 2006). Encourage participants to wear compression sleeves and to avoid any postures that result in arm pain. Initially, focus on increasing range of motion of the upper body with gentle shoulder stretches and chest-opening postures such as shoulder rolls, cactus arms, cow pose or a supported backbend. For strengthening exercises, provide modifications for postures that place a high percentage of the body weight into the arms, such as downward-facing dog, plank or low push-up position, until participants build strength in the upper body. Gradually progress as arm range of motion, strength and confidence improve.
- Peripheral Neuropathy: Peripheral neuropathy is a side effect of chemotherapy and can result in hand and foot numbness, muscle weakness and loss of balance (Wickham, 2007). Encourage participants with peripheral neuropathy to use a chair or stand close to the wall while performing standing or balance postures. If available, a chair yoga class may also benefit these participants.
- Include Meditation and Breathing: Be sure to incorporate both meditation and breathing exercises in your yoga classes and sessions, as both can be helpful in improving sleep, reducing stress and anxiety, managing pain and improving overall quality of life for your participants.
- Incorporate Postures for Strength and Physical Function: Because breast cancer treatments can result in losses in strength and physical function, focus on implementing postures and sequences that incorporate whole-body functional movements to build core stability and increase strength in the upper and lower body. Postures such as warrior I, warrior II, warrior III, high lunge, goddess, downward-facing dog and plank can promote whole-body strength and function
- Emphasize the Benefits of Each Posture: Educate your participants about the overall benefits of yoga and how breathing, meditation and the practice of specific postures can improve treatment-related side effects such as muscle weakness, pain, reduced shoulder flexibility, stress or anxiety. This can provide participants with the knowledge and confidence to perform these postures at home to help manage these side effects.
In addition to the special considerations above, teaching a yoga class for cancer patients or survivors requires additional knowledge and expertise. Therefore, if you are looking to teach or implement a cancer-specific yoga class at your facility, seek out additional cancer-specific yoga teacher trainings or become a Cancer Exercise Specialist through the American Council on Exercise.
References
Andysz, A. et al. (2014). Effect of a 10-week yoga programme on the quality of life of women after breast cancer surgery. Przegla?d Menopauzalny, 13, 3, 186–93.
Bower, J.E. et al. (2012). Yoga for persistent fatigue in breast cancer survivors: A randomized controlled trial. Cancer, 118, 15, 3766–3775.
Buffart, L.M. et al. (2012). Physical and psychosocial benefits of yoga in cancer patients and survivors, a systematic review and meta-analysis of randomized controlled trials. BMC Cancer, 12, 559.
Cramer, H. et al.(2016). Prevalence, patterns, and predictors of yoga use: Results of a U.S. Nationally Representative Survey. American Journal of Preventive Medicine, 50, 2, 230–235.
Culos-Reed, S.N. et al. (2006). A pilot study of yoga for breast cancer survivors: Physical and psychological benefits. Psycho-Oncology, 15, 10, 891–897.
Moadel, A.B. et al. (2007). Randomized controlled trial of yoga among a multiethnic sample of breast cancer patients: Effects on quality of life. Journal of Clinical Oncology, 25, 28, 4387–4395.
Sakorafas, G.H. et al. (2006). Lymphedema following axillary lymph node dissection for breast cancer. Surgical Oncology, 15, 3, 153–165.
Sehl, M. et al. (2013). Decline in physical functioning in first two years after breast cancer diagnosis predicts 10 year survival in older women. Journal of Cancer Survivorship, 7, 1, 20–31.
Simonavice, E. et al. (2011). Body composition, muscular strength, and physical function in breast cancer survivors. International Journal of Body Composition Research, 9, 2, 57–64.
Stasi, R. et al. (2003). Cancer-related fatigue: Evolving concepts in evaluation and treatment. Cancer, 98, 9, 1786–1801.
Warmuth, M.A. et al. (1998). Complications of axillary lymph node dissection for carcinoma of the breast: A report based on a patient survey. Cancer, 83, 7, 1362–1368.
Wickham, R. (2007). Chemotherapy-induced peripheral neuropathy: A review and implications for oncology nursing practice. Clinical Journal of Oncology Nursing, 11, 3, 361.
Want to make a significant impact on the health and well-being of countless yoga participants? Become an ACE Certified Group Fitness Instructor.
 by
by 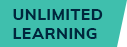






 by
by