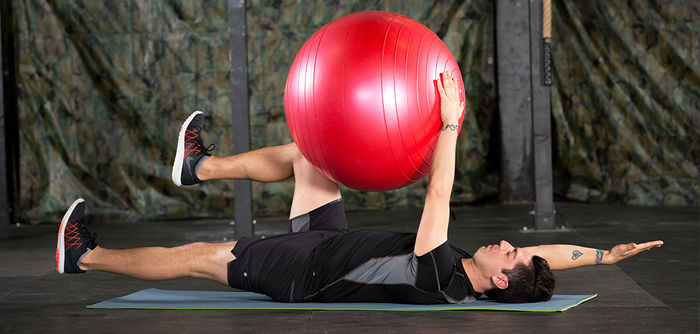
What Is Behavior Change and How Does It Relate to Physical Activity?

Becoming more physically active can be challenging, as countless factors influence your ability to move more. These behavior-change principles can help you make long-lasting changes to your lifestyle that will set you up for success.
Read More