
By Lance C. Dalleck, Ph.D.
According to recent data, only 21 percent of American adults meet federal physical activity guidelines for both aerobic and muscle-strengthening activities, with 32 percent reporting no leisure-time activity at all (Go et al., 2013). Physical inactivity is, of course, associated with numerous unhealthy conditions, including high cholesterol, hypertension, type 2 diabetes and atherosclerotic cardiovascular disease, and contributes to an estimated 250,000 premature deaths each year (Booth et al., 2000). Furthermore, millions of Americans currently take prescribed medications to try to manage these various chronic conditions.
Given these facts, it is inevitable that you will work with not only apparently healthy adults, but also chronic-diseased and medicated clientele. Therefore, it is essential that you understand how certain medications may affect your clients’ ability to exercise both safely and effectively. The following article takes a close look at five of the most common medications your clients may be taking and how they affect exercise. Armed with this knowledge, you will be able to design safe and effective exercise programs that meet the special needs and requirements of all your clients.
Figure 1. Percent of American Adults Taking Commonly Prescribed Medications Across Different Age Categories
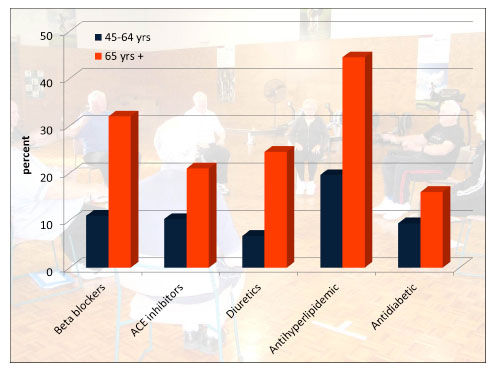
Created using data from the National Center for Health Statistics, 2012.
Prevalence of Prescribed Therapeutic Drugs
Current trends show that Americans are living longer, while the number of individuals living with chronic diseases continues to increase. In the past 100 years, life expectancy at birth in the U.S. increased from less than 50 years to more than 76 years. The U.S. Census Bureau has projected that by 2030, the number of adults 65 years of age and older will be approximately 70 million. Approximately 80 percent of individuals aged 65 years or older are living with at least one chronic health problem, and another 50 percent are living with two. Management of these chronic conditions involves numerous strategies including both lifestyle interventions (e.g., increased exercise and healthy eating) and the prescription of therapeutic drugs. Not surprisingly, the percentage of American adults taking medications for common chronic conditions (e.g., high cholesterol and/or hypertension) increases with age (Figure 1).
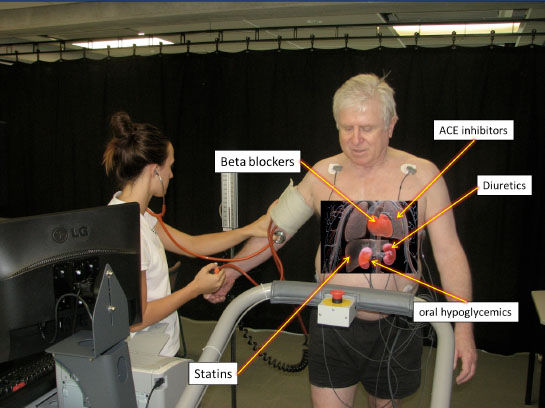
Figure 2. Location of Targeted Effect of Common Medications
1. BETA BLOCKERS
Mechanism of Action
Beta blockers are commonly prescribed medications for hypertension and heart disease. Beta blockers function by preventing the binding of epinephrine to receptors in the heart (Figure 2). This results in both decreased resting and exercise heart rate (HR) and blood pressure (BP) values. Commonly prescribed beta blockers include atenolol and metoprolol.
Interaction Between Medication and Exercise Response
The therapeutic effect provided by beta blockers also creates an altered physiological response to exercise. Beta blocker treatment blunts the usual increases in HR and BP that correspond to higher exercise intensities/workloads. Beta blockers can also cause glucose intolerance in people with diabetes by masking the symptoms of hypoglycemia.
Modifications Required in the Exercise Program
The fact that beta blockers attenuate the HR response to exercise means traditional methods for establishing target HR (e.g., peak HR method or HR reserve method) are likely to be invalid. Therefore, the most important program for individuals taking a beta blocker is to use an alternative method for setting target intensity. The ratings of perceived exertion (RPE) scale is an excellent option. And, because beta blockers can mask the usual symptoms of hypoglycemia in individuals with diabetes, strongly encourage your clients with diabetes who also are taking beta blockers to regularly check blood glucose values with their glucometers prior to exercise to ensure levels are in a safe range. Rechecking blood glucose values midway through an exercise session and/or at the conclusion of exercise to verify levels have remained in an appropriate range is also a good safety measure, especially early in a training program.
2. ACE INHIBITORS
Mechanism of Action
An ACE inhibitor (or angiotensin-converting-enzyme inhibitor) is a medication primarily used for the treatment of hypertension. Common ACE inhibitors include captopril, enalapril and lisinopril. ACE inhibitors reduce the activity of the complex renin-angiotensin-aldosterone system. Simply put, ACE inhibitors block the conversion of angiotensin I to angiotensin II primarily in the lungs (see Figure 2). The molecule angiotensin II is a potent vasoconstrictor of blood vessels. Therefore, reduced production of this molecule results in relaxation of the blood vessels and lower blood-pressure values.
Interaction Between Medication and Exercise Response
Individuals on ACE inhibitor medication have both lower resting and exercise blood-pressure values. However, it is the interaction between ACE inhibitors and the post-exercise blood pressure response that requires your additional attention. An acute beneficial response to exercise is a phenomenon known as post-exercise hypotension, whereby systolic blood pressure values can be reduced by 10 to 20 mmHg for up to nine hours after the conclusion of exercise. This occurs due to a persistent, but transient, relaxation of the blood vessels. The concern for individuals taking ACE inhibitors is that the combination of the reduction in blood pressure from the medication coupled with the naturally occurring post-exercise hypotension can result in excessive reductions in blood pressure. This can lead to untoward events such as dizziness and, in rare instances, syncope (i.e., temporary loss of consciousness).
Modifications Required in the Exercise Program
It is critical that clients who take ACE inhibitors consistently adhere to a gradual cool-down after each and every exercise session. One of the classic benefits of a cool-down is enhanced venous return and the prevention of blood pooling in the skeletal muscle. A gradual cool-down of five to 10 minutes of light aerobic activity permits the body to return to homeostasis and prevents excessive reductions in blood pressure.
3. DIURETICS

Mechanism of Action
Diuretic are another class of medications commonly used for the treatment of hypertension. One of the most common types of diuretics is hydrochlorothiazide (or HCTZ). Diuretics act on the kidney and lead to increased urine output (see Figure 2). An increase in urine excretion in turn leads to a lower plasma volume, which helps lower blood pressure.
Interaction Between Medication and Exercise Response
Much like clients who take ACE inhibitors, individuals on diuretics will have both lower resting and exercise blood-pressure values. It is important to note that ACE inhibitors and diuretics often are taken together. In this case, a principle concern is that the combination of the reduction in blood pressure from the ACE inhibitors and the diuretics, coupled with the naturally occurring post-exercise hypotension, can result in excessive reductions in blood pressure.
Modifications Required in the Exercise Program
Encourage your clients taking diuretics to unfailingly perform a gradual cool-down after all exercise sessions. It’s also a good idea to suggest your clients perform a daily weight check to ensure that the prescribed dosage of diuretic is continuing to have the desired effect (i.e., increased urine excretion-lowered plasma volume-reduced blood pressure). A sudden change in weight of a few pounds can help alert clients that something may be amiss and that they should get in touch with their physician.
4. STATINS
Mechanism of Action
Statins are the most commonly prescribed medication for high cholesterol. Statins function by inhibiting a key enzyme involved in the production of cholesterol in the liver (see Figure 2). Common statins include Lipitor, Zocor and Pravachol.
Interaction Between Medication and Exercise Response
Caution with regard to exercise is advised for individuals taking statins. Although not common, there are occasional instances where statins have been associated with exertional rhabdomyolysis. Rhabdomyolysis is a condition in which damaged skeletal muscle tissue breaks down and releases cellular content (e.g., protein myoglobin) into the blood that can be harmful to the kidneys. The incidence of exertional rhabdomyolysis is higher in deconditioned individuals performing high-intensity exercise, most notably resistance training and eccentric exercises. The condition is also likely to be exacerbated if the high-intensity exercise is also performed in hot, humid environments.
Modifications Required in the Exercise Program
Here are several preventative measures you can use to avoid help your clients who take statins to avoid exertional rhabdomyolysis:
- All exercise programming (aerobic and resistance training) should begin at low-intensity and progress gradually.
- Educate your clients about the signs and symptoms of exertional rhabdomyolysis, which may include muscle stiffness and/or pain, fatigue and dark-colored urine.
- Training sessions should be planned for cooler times of the day if exercise is to be performed outside.
- Encourage clients to always adequately hydrate before, during and after exercise.
5. ORAL HYPOGLYCEMICS
Mechanism of Action
Oral hypoglycemics are a class of medications commonly prescribed for individuals with type 2 diabetes. There are three major groups of oral hypoglycemics used to control blood glucose: 1) ß-cell stimulants for insulin release, 2) drugs to improve insulin sensitivity and 3) drugs that decrease intestinal absorption of carbohydrates. ß-cell stimulants function by inciting insulin release from the pancreas (see Figure 2). These medications are taken with meals and help alleviate excessive increases in post-meal blood glucose levels. The latter two oral hypoglycemic categories have little effect on the exercise response. A few common ß-cell stimulants include glipizide and glyburide.
Interaction Between Medication and Exercise Response
The transport of glucose from the blood into the muscle cell is facilitated by the transporter protein GLUT-4. These transporter proteins respond to two signals – insulin and exercise. Because of the insulin stimulation from ß-cell stimulants, when combined with exercise, there is increased potential for hypoglycemia (i.e., low blood glucose).
Modifications Required in the Exercise Program
The most important program modification for clients taking oral hypoglycemics is frequent monitoring of blood glucose values. Initially, this should include checking levels pre-exercise, at the mid-point of exercise and post-exercise. Once it has been established how much blood glucose values typically drop for a usual exercise session, and provided these changes in glucose levels are within an acceptable range, less-frequent monitoring will be required. It should be noted that it is not your responsibility to check blood glucose values. Rather, the client should bring his or her own glucometer and glucose strips, which are prescribed by a physician or endocrinologist.
References and Resources
American College of Sports Medicine (2013). ACSM’s Guidelines for Exercise Testing and Prescription (9th ed.). Baltimore, Md.: Lippincott Williams & Wilkins.
American College of Sports Medicine (2010). ACSM’s Resource Manual for Guidelines for Exercise Testing and Prescription (6th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins.
Booth, F.W. et al. (2000). Waging war on modern chronic diseases: primary prevention through exercise biology. Journal of Applied Physiology, 88, 2, 774–787.
Go, A.S. et al (2013). Heart disease and stroke statistics—2013 update: A report from the American Heart Association. Circulation, 127, e6–245.
National Center for Health Statistics (2011). Health, United States, 2011. Hyattsville, Md.
__________________________________________________________________________

Lance C. Dalleck, Ph.D., is academic coordinator of the cardiac rehabilitation postgraduate program at the University of Auckland in New Zealand. His research interests include improving exercise performance and health outcomes through evidence-based practice, quantifying the energy expenditure of outdoor and non-traditional types of physical activity, and studying historical perspectives in health, fitness and exercise physiology.