With physical activity, the possibility of injury is always present. Damage to the skin, blood vessels, nerves and viscera occur simultaneously when the bone, ligaments, cartilage and/or muscles are damaged. Designing safe and effective programs for injured clients requires a basic knowledge of common musculoskeletal injuries, and referring clients to the qualified healthcare professional when necessary.
Here are some of the more common musculoskeletal injuries you might see in your work as a fitness professional:
Muscle tendinitis results from muscles working beyond their capacity, causing tears in the muscle fibers. There may be tightness or tension, mild tears or pain, weakness, swelling, discoloration and, in more severe cases, loss of function. Injury primarily occurs in larger muscle groups of the lower extremities such as the hamstrings, groin and calf.
Ligament sprains are most often due to trauma at joints such as the ankle, knee and thumb /finger, and shoulder. There may be pain, swelling and instability, decreased range of motion and loss of function at the site of injury.
Overuse conditions include tendinitis, bursitis and fasciitis, and are caused by inflammation of the tendon, bursa sac and fascia (connective tissue). Tendinitis is diagnosed most often in the shoulder, elbows, knees and ankles. Bursitis, repetitive stress, muscle imbalance or muscle tightness on top of the bursa can affect the shoulders, hips and knees. Fasciitis most commonly occurs at the bottom or back of the foot.
Cartilage damage most often affects the knee. Usually damage occurs to the hyaline (covers the knee), menisci (absorbs shock in the knee), and behind the patella (the knee cap)
Bone fractures are caused by either low-impact trauma such as a fall or repeated microtrauma to bone, resulting in stress fractures, or by high-impact trauma, such as motor accidents or high-impact sports such as football.
Whether the injury is preexisting or acute, how do you safely respond to an injured client?
When approached by clients regarding preexisting injury, it is essential that you remain within your scope of practice and refrain from diagnosing the injury. Medical history and a proper assessment will help you decide whether the client is ready for exercise or should seek physicians’ clearance. With preexisting injuries, it may be necessary to modify the client’s exercise program.
Acute injuries, however, must be handled differently. Immediate attention, with caution, is required. Provide assistance using P.R.I.C.E.:
• Protect the injured site
• Rest or Restrict, especially weight-bearing activity
• Ice until swelling has passed
• Compression at site to minimize swelling
• Elevation of injured area
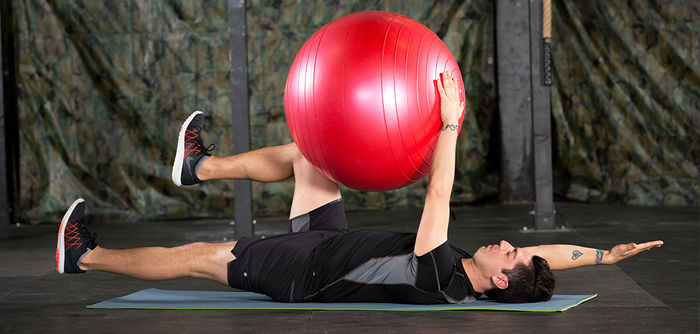
The previously mentioned strains and injuries have been associated with decreased flexibility in the muscle. The shortened state of the muscle prevents proper force generation. This weakened and inflexible state often leads to injury. Therefore, you need to be cautious in recommending flexibility exercises. Here are the relative and absolute contraindications to stretching.
Relative contraindications include:
• Pain in the affected area
• Restrictions from the client’s doctor
• Prolonged immobilization of muscles and connective tissue
• Joint swelling (effusion) from trauma or disease
• Presence of osteoporosis or Rheumatoid Arthritis
Absolute contraindications include:
• A fracture site that is healing
• Acute soft-tissue injury
• Post-surgical conditions
• Joint hypermobility
• An area of infection
When designing exercise programs, the utmost care must be taken to modify programming according to any types of injury the client may have experienced. Furthermore, clients should be educated on avoiding activities that aggravate the injury. Emphasis should be placed on improving posture, as well as regaining strength and flexibility at the injured site.
 by
by 











 by
by