In an “ideal world,” health professionals would provide sound information to their patients or clients about their health behaviors, such as exercise and healthy eating, and that would be all those individuals would need to affect lasting behavior change. Although there are notable exceptions, that is not what typically occurs. This is especially the case when clients’ goals are related to reducing their weight. Nearly 75% of the U.S. adult population is at a body mass index high enough to be associated with increased health risks. In addition,?it's?worth noting that?in?determining?the number of Americans who attain the recommended minimum of 150 minutes of weekly moderate-intensity exercise, one piece of?research?found that?only?6 to 8% of adolescents and 5% of adults?do so, while another?study?put that number?at 10% for adults.?
Clearly, there are additional tasks for health professionals, including ACE Certified Health Coaches and Exercise Professionals, to take on, beyond simply providing sound advice. For example, symptoms of anxiety and/or depressive disorders are now present in one-third of U.S. adults, which means this ought to be a primary concern for all involved. In this blog, I explore methods that can be incorporated into your practice to address changes in health behaviors that will help your clients reach their health-related goals, whether those pertain to physical or mental health.
A considerable amount of work done by me and other health psychologists is unrelated to the classical health-related education often shared with clients. Most of us acknowledge the large-scale lack of connection between how much an adult knows about diet and exercise and their behaviors. Therefore, we are concerned with fostering behavioral changes that are resilient. Because 50 to 60% of adults starting or restarting an exercise program are predicted to drop out within several weeks or months, and regain of lost weight (sometimes beyond baseline weight) is highly predictable beyond an initial six to nine months of the weight loss, these efforts are worthwhile.
The good news is that while attaining 150 minutes of weekly exercise is a laudable goal, the performance of far less exercise is associated with substantial impacts on anxiety and depression. Additionally, research suggests that while increased exercise is associated with controlled eating and weight loss, frequency of moderate-intensity bouts of exercise (of at least 15 minutes each) does not matter very much, as long as a two session per week are consistently met.
Then, what is it about exercise that is associated with such changes, because it clearly is not calorie burn (or more exercise would have been associated with more weight loss in our samples of adults with obesity)? Excluding the super-fit, the findings imply that when exercise is successfully undertaken, a certain amount of self-regulation through common lifestyle barriers (e.g., slow results, physical discomfort, boredom and body-image anxiety) is required. As suggested in coaction theory (which refers to the extent to which taking one action on one behavior increases the odds of taking action on a second behavior), some of that self-regulation carries over to controlled eating and weight loss. Also, maintaining exercise is associated with better mood, which, in addition to enhanced self-regulation, helps control emotional eating (an important issue for many). However, while some of this “transfer” of self-regulation spontaneously carries over from an exercise context to a controlled eating context, when that process is supported by a knowledgeable health professional, the effects can be greatly enhanced.
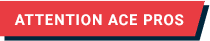
There are several other behavioral theories that can help shape the practice of an effective health professional. For example, self-regulation theory suggests that if individuals rehearse self-regulatory skills such as (1) reframing negative self-talk, (2) planning for slips in their routine, (3) documenting short-term goals, (4) progress tracking and (5) attentional control, those skills will become more robust and transfer more effectively from one context (e.g., exercise) to another (e.g., controlled eating).
Social cognitive theory also acknowledges the value of carefully building self-regulation skills, but it focuses more on the increased competency one will feel (i.e., self-efficacy) in overcoming barriers/challenges that were previously associated with failure. Self-efficacy is associated with ongoing effort and goal commitment. Because exercise volume is not associated with mood improvements (i.e., there is no exercise dose–mood improvement effect), it has been suggested that this increase in self-efficacy promotes improvements in anxiety and depression. Keeping exercise amounts manageable is also associated with adherence.
If health coaches and exercise professionals, along with other health professionals, increasingly perceive themselves as experts in supporting behavior-change as much as information-exchange experts, their contact time with clients will look different. Rather than focusing on the highly motivated, they will have expertise applicable to the typical U.S. adult who may struggle with health behavior changes. They will also open their practices up to those with health risks that require attention in a more complete, holistic manner. In future blogs, I will provide greater detail on specific self-regulatory skills and strategies and explain how you can use them to empower your clients.
 by
by