The Real Reason So Many People Are Overweight

A new study places the blame for skyrocketing rates of obesity in the U.S. on widespread inactivity rather than excessive caloric intake. So, while no one’s arguing that supersized portions are good for us, it appears that sedentary lifestyles are largely responsible for so many people packing on the pounds.
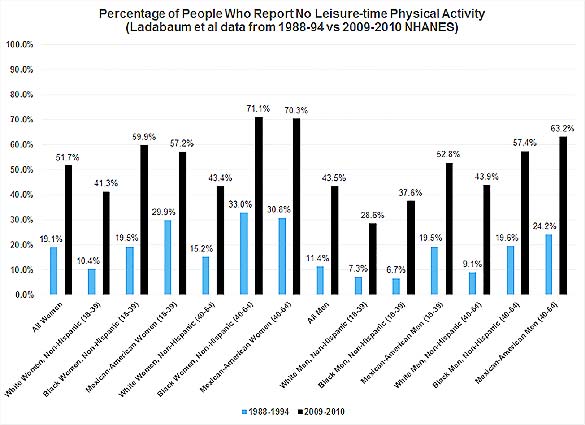
The study, published in The American Journal of Medicine, analyzed data from the well-known National Health and Nutrition Examination Survey (NHANES), a program of studies designed to assess the health and nutritional status of adults and children in the United States. Researchers discovered that in the past 20 years there has been a sharp decrease in physical exercise and an increase in average body mass index (BMI), while caloric intake has remained steady. Investigators theorized that a nationwide drop in leisure-time physical activity, especially among young women, may be responsible for the upward trend in obesity rates. For example, the number of U.S. adult women who reported no physical activity jumped from 19.1 percent in 1994 to 51.7 percent in 2010. For men, the number increased from 11.4 percent in 1994 to 43.5 percent in 2010. During the period, average BMI has increased across the board, with the most dramatic rise found among young women ages 18 to 39.
“These changes have occurred in the context of substantial increases in the proportion of adults reporting no leisure-time physical activity, but in the absence of any significant population-level changes in average daily caloric intake,” explains lead investigator Uri Ladabaum, M.D., M.S., Associate Professor of Medicine (Gastroenterology and Hepatology), Stanford University School of Medicine. “At the population level, we found a significant association between the level of leisure-time physical activity, but not daily caloric intake, and the increases in both BMI and waist circumference.”
It is significant to note that, while investigators did not examine what types of foods were consumed, they did observe that total daily calorie, fat, carbohydrate and protein consumption have not changed significantly over the last 20 years, yet the obesity rate among Americans is continuing to rise.
Researchers also tracked the rise in abdominal obesity, which is an independent indicator of mortality even among people with normal BMIs. Abdominal obesity is defined by waist circumference of 34.65 inches (88 cm) or greater for women and 40.16 inches (102 cm) or greater for men. Data showed that average waist circumference increased by 0.37 percent per year for women and 0.27 percent per year for men. Just like the rise in average BMIs, the group most affected by increased rates of abdominal obesity was women.
“The prevalence of abdominal obesity has increased among normal-weight women and overweight women and men,” observes Dr. Ladabaum. “It remains controversial whether overweight alone increases mortality risk, but the trends in abdominal obesity among the overweight are concerning in light of the risks associated with increased waist circumference independent of BMI.”
When Ladabaum and his research team grouped respondents tothe most recent NHANES survey by race/ethnicity and age, they found that more than 50 percent of the workforce-aged adults in eight demographic subgroups reported no leisure-time physical activity. Table 1 displays the results and highlights the differences between the 1994 survey results and those collected in 2010 (albeit, with slightly different survey methods). According to this data, women—black and Mexican-American women in particular—showed the greatest decreases in reported exercise.
Table 1
While increased caloric intake is often blamed for rising rates of obesity, no association between these was found in this study.
“Our findings do not support the popular notion that the increase of obesity in the United States can be attributed primarily to sustained increase over time in the average daily caloric intake of Americans,” concludes Dr. Ladabaum. “Although the overall trends in obesity in the United States are well appreciated and obesity prevalence may be stabilizing, our analyses highlight troublesome trends in younger adults, in women, and in abdominal obesity prevalence, as well as persistent racial/ethnic disparities.”
Dr. Natalie Digate Muth, ACE's Healthcare Solutions Director, is not ready to write off the impact of caloric intake on obesity just yet. "While it is interesting that the paper found no association between caloric intake and BMI, it is well established that changes to dietary intake have played a substantial role in contributing to the obesity epidemic. We must take these results to the contrary with a grain of salt,” urges Digate Muth. “The measures of nutritional intake were self-reported and the reliability of calorie count through such measures is questionable.”
What Do These Findings Mean For Fitness Professionals?
The United States suffers not only from an epidemic of obesity, but from an epidemic of physical inactivity as well. “This paper serves to highlight this alarming reality and issue a call to action to go beyond to pushing the recommendation for all Americans to get 150 minutes of physical activity per week, to creating systemic changes to support the routine integration of physical activity in every American’s life,” says Digate Muth. “If we do not, we cannot expect to make progress in the obesity epidemic or in improving the overall health of Americans.”
Fitness professionals are uniquely positioned to take a leading role in the shift from a largely sedentary population to one that moves more—even if not enough to meet guidelines. After all, with about half of the population reporting no leisure time physical activity, even the smallest improvements will add up. But in order to do this, the industry must reach beyond those people who already have active lives. Through partnerships with workplaces, physicians and healthcare systems, schools, insurers, and even city planners, fitness professionals can help develop strategies and programs to help make physical activity a routine, enjoyable part of people’s everyday lives, especially among those at highest risk of physical inactivity.
While there is no easy answer in America’s ongoing battle against obesity, identifying the link between the drop in physical activity and increased BMIs, as well as the groups particularly affected, can assist public health officials to develop targeted, effective interventions. In an accompanying commentary Pamela Powers Hannley, M.P.H., Managing Editor, The American Journal of Medicine, notes, “If we as a country truly want to take control of our health and our healthcare costs, [this study] should be our clarion call. From encouraging communities to provide safe places for physical activity to ensuring ample supply of healthy food to empowering Americans to take control of their health, we must launch a concerted comprehensive effort to control obesity.”
Sources
Hannley, P.P. (2014). Move more, eat less: It’s time for americans to get serious about exercise. The American Journal of Medicine.
Ladabaum, U. et al. (2014). Obesity, abdominal obesity, physical activity and caloric intake in U.S. adults: 1988 to 2010. The American Journal of Medicine.
More Articles
- ProSource™: August 2014
ACE Study Reveals Best Biceps Exercises
- ProSource™: August 2014
Can You Train Upper and Lower Abs Separately?
Health and Fitness Expert
- ProSource™: August 2014
Creating a Profitable Nutrition and Weight-loss Challenge
Contributor
- ProSource™: August 2014
14 Tips for Marketing Your Fitness Brand on Social Media
Health and Fitness Expert
- ProSource™: August 2014
5 Tech Tools to Enhance Your Fitness Business (and Increase Your Bottom Line)
Health and Fitness Expert