Historically, reduced levels of physical activity was recommended for women during pregnancy due to concerns that exercise could negatively affect pregnancy outcomes (e.g., poor fetal growth, premature delivery, miscarriage, and musculoskeletal injury). However, these concerns have not been substantiated and recommendations by The American College of Obstetricians and Gynecologists (2020) suggest that during pregnancy, exercise is safe and desirable, but excessive weight gain and physical inactivity in pregnancy is now recognized as independent risk factors for maternal obesity and related pregnancy complications.
Currently, pregnant women are encouraged to accumulate a minimum of at least 150 minutes of moderate-intensity aerobic activity on most—if not all—days of the week in the absence of medical or obstetric complications and to participate in muscle strengthening activities during and after pregnancy. In fact, during pregnancy exercise recommendations are the same as those for the general population.
It is important to consider that during pregnancy is an ideal time for behavior modification and making lifestyle changes because of access to increased medical supervision and motivation to improve health. Adhering to the tenets of the ACE Mover Method and following the ACE ABC approach can allow health coaches and exercise professionals to collaborate with clients to create a truly personalized experience. If a woman is new to exercise during pregnancy, they may need to set goals for working up to 20 to 30 minutes of moderate-intensity exercise and may achieve health benefits based on the accumulated volume of physical activity. In other words, bouts of activity of any duration contribute to health benefits.
Pre-activity Screening
The Canadian Society for Exercise Physiology has created a screening tool called the Get Active Questionnaire for Pregnancy to help exercise professionals and health coaches decide if women should speak to their Obstetric health care provider before beginning or continuing to be physically active during pregnancy. This resource provides a convenient checklist for the evaluation of women during pregnancy with an interest in beginning or maintaining an exercise program throughout their pregnancy.
General Exercise Recommendations for Women During Pregnancy
Collaborating with women during pregnancy to set realistic goals may help them to focus on self-efficacy, enjoyment, and finding success, while working to accumulate specific exercise recommendations. Although there are many benefits to beginning or maintaining an exercise program during pregnancy (e.g., improving or maintaining physical fitness, reduced risk of gestational diabetes mellitus, cesarean birth, operative vaginal delivery, postpartum recovery time, bodily pain, lumbar and sciatic pain, pain disability, depressive disorder in the postpartum period, excessive weight gain, anxiety, heartburn, insomnia, and leg cramps ,), it may still be important for women during pregnancy to receive a thorough clinical evaluation before starting a new exercise program. Both the ACOG (2020) and ACSM (2022) recommend that a clinical evaluation take place before beginning an exercise program and that recommendations for exercise should be provided in consultation with the client’s health care provider.
In the absence of any contraindications, pregnant women who have uncomplicated health pregnancies are encouraged to participate in regular, moderate-intensity physical activity [e.g., zone 1, below VT1 (can talk comfortably), RPE of 3–4 on the 0–10 scale or 12–13 on the 6–20 scale, and 3–5.9 METs]. In addition, women who participated in regular exercise prior to pregnancy can maintain pre-pregnancy intensity levels but may need to be more mindful of pre-exercise caloric intake to avoid hypoglycemia or decrease the length of the exercise session.
Examples of moderate-intensity physical activity include:
- Walking
- Aquatic exercise
- Stationary cycling
- Yoga
- Pilates
- Muscle Strengthening (e.g., using weights, elastic bands)
- Racquet sports
- Low-impact aerobics
Examples of exercises that should be avoided during pregnancy include:
- Contact sports (hockey, boxing, soccer)
- Activities with a high risk of falling (gymnastics, horseback riding, off-road cycling)
- Scuba diving
- Surfing
- Hot yoga
- Sky diving
- Activities performed above 6,000 feet (if you do not already live at high altitude)
It is important that health coaches and exercise professionals are aware of warning signs to discontinue exercise. If any of the following warning signs occur, exercise should be discontinued until the condition can be discussed with their physician or obstetric care provider.
Warning Signs to Discontinue Exercise While Pregnant:
· Abdominal pain
· Vaginal bleeding
· Regular painful contraction
· Amniotic fluid leakage
· Dyspnea before exertion
· Dizziness
· Headache
· Chest pain
· Muscle weakness affecting balance
· Calf pain or swelling
To assist health coaches and exercise professionals in creating safe and effective exercise programs for women during pregnancy, the American College of Obstetricians and Gynecologists (2020) and the US Department of Health and Human Services(2018) has established specific recommendations for safe and effective exercise during pregnancy. The table below summarizes these recommendations.
|
FITT |
Aerobic |
Resistance |
|
Frequency |
At least 3-4 days per week |
At least 2 days per week |
|
Intensity |
-Moderate (12-14 on the 6-20 Borg scale) -60-80% of age predicted maximum maternal heart rate |
Do activities that make your muscles work harder than usual
8-12 repetitions |
|
Type |
|
Free weights, elastic bands, body weight, weight machines |
|
Time |
30-60 minutes |
1-3 Sets |
|
OTHER FACTORS |
|
|
|
-Environment
-Supervision
-When to end |
Thermoneutral or controlled
Preferred, if available
Until delivery (as tolerated) |
|
Exercise Guidelines for Women During Pregnancy
Women who have been previously active may continue their exercise program. The upper level of safe exercise intensity has not been established. ACOG (2020) guidelines state that women with healthy uncomplicated pregnancies should be able to maintain their previous level of exercise intensity, as tolerated.
Women who have not previously been physically active should begin slowly and progress to a moderate level of exercise. Some women may need to begin with low intensity and shorter durations (<10 minutes) and/or perform intermittent activity. Using the talk test will ensure a more effective means than heart rate to monitor exercise intensity. Staying below the first ventilatory threshold (VT1) indicates a moderate level of cardiorespiratory intensity.
Avoid activities with high risk of abdominal trauma from contact or fall (e.g., contact sports, skiing, and surfing). In addition, exercise performed in extreme heat (e.g., “hot” yoga) should be avoided. Certain exercises (e.g., jogging, running, racquet sports, and muscular training) may be safe to initiate or continue with during pregnancy, while other activities may need to be modified or discussed with an obstetric care provider before participation.
Focus on hydration and balancing caloric intake with the metabolic demands of exercise and pregnancy.
Some pregnant women may benefit from a small snack prior to exercise to help avoid hypoglycemia, especially when exercising at a moderate intensity for longer than 45 minutes.
Consider recommending shorter sessions (e.g., 30 minutes versus 60 minutes) for new clients who have not exercised before pregnancy and then slowly increase duration and intensity over the course of the program.
Choose exercises to support the changing COG, such as squats, stiff-legged deadlifts, side lunges, lat pull-downs, seated rows, and bird dog exercises.
Encourage clients to discuss their energy level, aches and pains, and exercise warning signs in real time so the program can be modified accordingly. Individualize intensity level and rest time as needed. These requirements may change daily.
Those who are pregnant should avoid standing still or lying flat on their backs for long periods. These positions may cause blood pressure to decrease for a short time.
Avoid bouncy, jerky, and high-impact movements that can increase your risk of being hurt.
Exercise During the Postpartum Period
Returning to physical activity after pregnancy also has benefits (e.g., improved maternal cardiorespiratory fitness without affecting milk production or composition of infant growth) and is associated with decreased incidence of postpartum depression. Although some recovery time to regain strength is required, during the initial six weeks following delivery your client could begin to slowly increase physical activity as a means of relaxation, personal time, and regaining a sense of control. Women who are lactating should also consider feeding their infants or expressing milk prior to exercise to avoid discomfort.
The following guidelines should be followed during the Postpartum Period:
Obtain physician clearance and/or guidelines prior to resuming or starting an exercise program depending on the mode of delivery and if medical or surgical complications are present.
Begin slowly and gradually increase duration, frequency, and then intensity. Depending on their personal goals and energy levels, women may increase their activity levels until moderate-intensity activity or pre-pregnancy activity levels have been met, with an eventual goal of achieving at least 150 minutes of moderate intensity activity per week.
ACOG (2020) recommends exercises to strengthen major muscle groups. A woman may progress in activity as she feels ready and as her physician recommends.
Drink plenty of water before participating in physical activity and consider expressing milk before exercise to avoid discomfort from engorged breasts.
For more details regarding exercise program design and pregnancy, click on the article links below:
Training the Late-term Prenatal Client
Help Your Pregnant Clients Exercise Safely Through the Summer Months
Prenatal fitness modifications
References
American College of Obstetricians and Gynecologists. (2020). ACOG Committee Opinion. Washington, DC: American College of Obstetricians and Gynecologists. Retrieved from https://www.acog.org/-/media/project/acog/acogorg/clinical/files/committee-opinion/articles/2020/04/physical-activity-and-exercise-during-pregnancy-and-the-postpartum-period.pdf
American College of Sports Medicine (2022). ACSM’s Guidelines for Exercise Testing and Prescription (11th ed.). Philadelphia: Wolters Kluwer/Lippincott Williams & Wilkins.
Shroyer, L.. (2020). Exercise Considerations Across the Lifespan. In B. C. Editor, J.S. editor, & G.D Editor (Eds.), ACE’s The Exercise Professional’s Guide to Personal Training Manual (652-675). San Diego, CA: American Council on Exercise.
 by
by 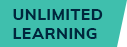





 by
by