Prescription for Activity Task Force: The Systems-change Map
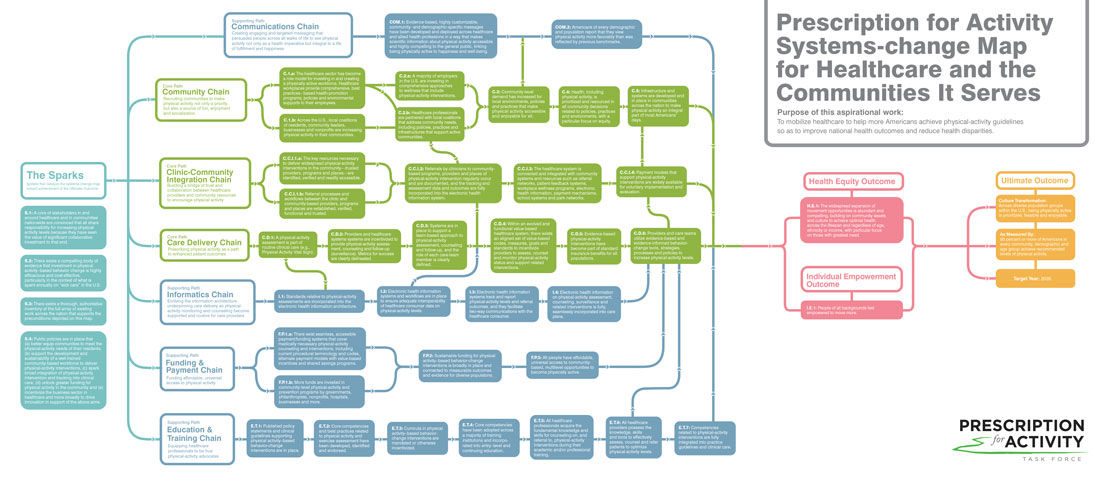
In our previous article on the Prescription for Activity (PfA) Task Force, we introduced the organizations and people involved and explained the process they used to develop a systems-change map that will enable more people in the U.S. to achieve the many benefits of a physically active lifestyle. In addition, we revealed the Ultimate Outcome that serves as the guiding principle for their ongoing work:
Culture Transformation:
Across diverse population groups within the U.S., being physically active is prioritized, feasible and enjoyable.
As Measured By:
50 percent or more of Americans in every community, demographic and age group achieve recommended levels of physical activity.
Target Year:
2035
In this article, the second of a three-part series, we walk you through the various elements that make up the PfA Task Force’s systems-change map and show how they work collaboratively to build toward the achievement of the Ultimate Outcome by 2035.
As you read through the summary of each chain presented in this article, take a few minutes to review the elements that make up that chain in the systems-change map. Doing so will give you the opportunity to understand the sequential outcomes that the Task Force members feel are necessary to steadily build toward the achievement of the Ultimate Outcome by 2035.
While the Ultimate Outcome appears at the “end” of the systems’ change map, it was the starting point for the theory of change strategic planning process, as explained in the first article in this series. While the map moves from left to right, the thinking behind it moved from right to left, which means that the Task Force began by looking at the big picture and then worked to figure out exactly what needed to take place, and in what sequence, to achieve that Ultimate Outcome.
Health Equity
The first topic discussed by the PfA Task Force was health equity as a prerequisite to all of the work that follows. Health equity is not only an outcome of this work, but also a lens through which each of the component chains of the map, and all of the outcomes that fall within those chains, are viewed.
The pursuit of a more physically active America, and the belief that every American must have a fair chance to achieve his or her best health, are fundamentally intertwined. Health equity exists when everyone has the opportunity to fulfill his or her full health potential, and when no one is at a disadvantage from doing so because of social position or any other circumstance. Unfortunately, that is not currently the case in America, as the burdens of ill health and the benefits of good health are inequitably distributed. As healthcare evolves to expand its capacity to help vastly more Americans achieve recommended physical-activity levels, the compelling opportunities to become physically active that emerge must be equitable across age, ethnicity and socioeconomic status.
Individual Empowerment
The PfA Task Force recognizes that individual empowerment is an essential step between creating the opportunity for people to be active and realizing a culture of activity where at least 50 percent of people from all backgrounds achieve activity recommendations.
People will move more when they have ample opportunities to be active in an enjoyable and safe way as part of their daily lives; believe in the benefits and rewards of a physically active lifestyle; feel ready and able to take the first steps; and feel supported by their loved ones, workplaces, communities, and trusted community resources such as healthcare providers and their teams.
The Core Path
To achieve Health Equity, Individual Empowerment and the Ultimate Outcome, the PfA Task Force developed a Core Path that includes a care delivery chain, a community chain and a clinic-community integration chain that come together to create a healthcare system in which providers routinely assess physical-activity levels for all patients, help those patients most in need develop a plan to optimize activity, and seamlessly refer patients to opportunities for community-based physical activity. Community-based organizations support the healthcare system with ample and equitable physical-activity opportunities, and share progress and outcomes with healthcare partners.
Care Delivery Chain
An evolution of healthcare delivery is essential, such that clinicians across healthcare assess, prescribe and monitor patients’ physical activity. This process should become as integral to the clinical experience as tracking weight change or measuring blood pressure. The systems that guide and support clinical work—standards of care, best practices, information architecture, protocols, benefit structures and the like—must evolve to support and incentivize that goal. In addition, priority should be placed on creating opportunities and incentives for clinical staff to model adoption of a physically active lifestyle. While the epidemic of physical inactivity will not be solved in the doctor’s office, with concrete steps the clinic can become a catalyst for creating more active populations.
Community Chain
The PfA Task Force calls for all communities to become pivotal purveyors, translators and celebrators of physical activity, helping their members understand and contextualize the necessity and profound benefit of becoming and staying active. Becoming physically active cannot be a mandate. It must be a cultural priority in all communities, and that requires community leaders to help members associate regular physical activity with joyful living as part of rich community life. Communities must create safe and compelling places to get and stay active, which will require local coalitions that include residents as active participants.
Clinic-Community Integration Chain
For healthcare to realize its full potential as a catalyst to help vastly more Americans meet physical-activity guidelines, the traditional “wall” between the clinic and surrounding communities must be lowered. Physical activity–based behavior-change interventions must become affordable and widely available directly in the community as an extension of clinical care. Interventions prescribed and monitored by the clinic must be delivered beyond clinic walls by members of an extended care team who meet people directly where they are—in the home, at school, at work and even in places of worship. To accomplish these goals, the clinic and the community-based providers and programs surrounding the clinic must become seamlessly linked. Referrals must take place, trust must be high and information architecture must be secure. Finally, the behavior-change interventions delivered in the community must be as important to the overall plan of care as the care administered in the examination room.
The Supporting Chains
The efforts reflected in the Care Delivery, Community and Clinic-Community Integration Chains are supported through education and training of providers and allied health professionals, funding and investment from stakeholders and partners, health informatics and communication supports.
Education and Training Chain
Regular physical activity is a potent medicine that should be widely prescribed to prevent and treat a long list of chronic diseases, as well as to promote optimal health and quality of life. In order to make this possible, education on the importance of physical activity to overall health, as well as on how to guide someone through a safe and effective exercise program, must be incorporated into the curricula for all health professionals. For physicians, education should be ongoing, beginning in medical school, continuing through residency and throughout one’s career via continuing medical education. In fact, this paradigm should be integrated into the curricula of all healthcare professions (e.g., nursing, physical therapy, dentistry and pharmacy). All healthcare professionals should have the educational training that would allow them to competently discuss the importance of exercise and physical activity with all of their patients. The healthcare professionals with whom consumers interact every day must become equipped to understand, recommend, support and track physical-activity interventions.
Funding and Payment Chain
Increased physical-activity levels lead to improved health outcomes, which lead to reduced healthcare costs, increased healthy days, reduced sick days and higher productivity. For these reasons, the PfA Task Force calls for the unleashing of significant investment in diverse, affordable and compelling physical-activity opportunities. While the PfA Task Force calls for growing the evidence base linking physical-activity interventions with reduced costs and enhanced patient and provider experiences, it believes that broad-scale funding of physical activity could return billions of dollars to the U.S. economy and significantly advance health equity.
Informatics Chain
Health information architecture must equip the sector to become a motivator of physical activity across income levels, ethnicities, age and other boundaries. The PfA Task Force calls for the development, acceptance and widespread use of standards for how physical activity is defined across the information architecture that increasingly underpins healthcare delivery. Providers must more seamlessly assess, counsel and monitor physical-activity levels. Currently, that happens only when there is a consistent, reliable way to enter, access and analyze the data. Workflows must be created and put in place, consistency and functionality across the entire healthcare system must be achieved and analytics must be robust.
Communications Chain
Thoughtful and effective communications, carefully tailored to audiences across communities, demographics and ages, will be key to many of the preconditions in the systems-change map. Thus, communications could have been woven into each of the chains where it will play a role. However, the PfA Task Force determined that communications, because of its extreme importance, warrants its own distinct path of work. Without a fundamentally new message about physical activity that persuades people across all walks of life to see physical activity not only as a health imperative but also as enjoyable and integral to a better quality of life, a significant number of preconditions across the entire systems-change map will not be realized.
The Sparks
Along the left side of the systems-change map are the Sparks, which are the earliest preconditions upon which the transformation suggested by the systems-change map are set into motion. They include (1) critical-mass belief in the power of investment in a more physically active population, (2) evidence that physical activity–based behavior-change interventions improve health outcomes while reducing healthcare costs and (3) policies that make it easy and compelling to invest and innovate in service of a more active America. The “Spark” preconditions are the initial stepping-stones toward a future in which vastly more Americans meet physical-activity guidelines, a culture that values such priorities and a healthcare system that plays a significant role in catalyzing those changes.
What’s Next
In part 3 of this series, we look at the key next steps that the PfA Task Force has identified as the starting points for implementation of the vision illustrated by the systems-change map. Importantly, you will learn where you, as an exercise professional or health coach, fit into this long-term vision.

More Articles
- Certified™: February 2018
ACE-SPONSORED RESEARCH: What Is the Best Exercise for the Hamstrings?
Contributor
- Certified™: February 2018
StrongBoard: An ACE Integrated Fitness Training® Model-based Workout
Health and Fitness Expert
- Certified™: February 2018
Total-body Sprint/Body-weight Circuit to Improve Muscular Endurance
Health and Fitness Expert
 by
by